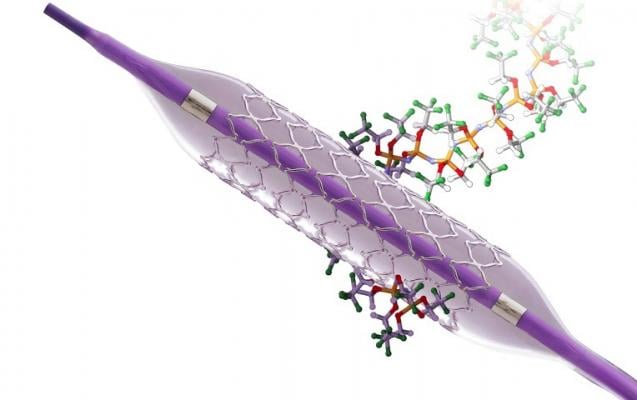
October 22, 2020 – For patients undergoing percutaneous coronary intervention (PCI), treatment with the nanotechnology polymer-coated Cobra PzF stent plus 14-day dual anti-platelet therapy (DAPT) did not reduce bleeding or establish non-inferior outcomes for thrombotic events compared with a drug-eluting stent (DES) and standard three or six-month DAPT therapy.
Findings were reported at the 2020 Transcatheter Cardiovascular Therapeutics (TCT) Connect virtual meeting.
“In patients undergoing PCI for acute or chronic coronary syndromes who are receiving oral anticoagulation with or without dose reduction, stenting with Cobra PzF stents with 14 days DAPT did not reduce BARC 2-5 bleeding and did not meet non-inferiority criteria with respect to thrombotic events compared with standard DES and 3-6 months of DAPT,“ said Robert A. Byrne, MB BCh, Ph.D. Dr. Byrne is director of cardiology, Mater Private Hospital, Dublin and chair of cardiovascular research, Royal College of Surgeons in Ireland. “Treatment with the Cobra PzF stent was safe with ST rates considerably lower than those seen in earlier trials with HBR patients despite DAPT duration of only 14 days.
The COBRA-REDUCE trial was a randomized, open-label, active-controlled, assessor-blinded, multi-center trial. A total of 996 patients were enrolled between February 2016 and May 2020 at 59 sites in Europe and the United States. Patients at high bleeding risk (HBR) due to requirement for oral anticoagulation were randomized at the time of PCI to treatment with the COBRA-PzF stent followed by a very short duration (14 days) of DAPT or an FDA-approved new generation DES followed by guideline-recommended DAPT duration (three or six months).
The primary endpoints were BARC class ≥ 2 bleeding beyond 14 days or after hospital discharge (whichever is later) at six months post-randomization and composite of death, myocardial infarction (MI), definite/probable stent thrombosis (ST), or ischemic stroke at six months.
Secondary endpoints included composite endpoint of all cause death, MI, definite/probable ST, ischemia-driven TLR, or ischemic stroke; composite of cardiac death and MI; ischemia driven TLR; definite/probable ST; ischemic stroke; BARC class 3-5 bleeding; TIMI major bleeding; TIMI major or minor bleeding; and health economic utilities.
The rate of bleeding in the test group (COBRA-PzF stent with short DAPT) was 7.5 % and in the control group (DES with standard DAPT) was 8.9% (p=0.477). The rate of the composite thrombotic endpoint was 7.7% in the test group and 5.2% in the control group (Difference +2.5% (95% CI 5.15%), p non-inferiority=0.061).
“Ongoing follow-up and planned analysis of secondary outcomes at 12 months is needed to assess comparative efficacy of the treatment arms in relation to the study devices. Analyses of bleeding events according to medication compliance, OAC dose, and number of ARC-HBR criteria will permit examination of interaction between treatment effect, anticoagulation intensity and baseline bleeding risk,” Byrne said.
The COBRA-REDUCE trial was funded by CeloNova Biosciences. Byrne reported the following disclosures: Research contract with institution of prior employment: CeloNova Biosciences.
Find additional TCT 2020 news, video and late-breaking studies


 January 05, 2026
January 05, 2026 









