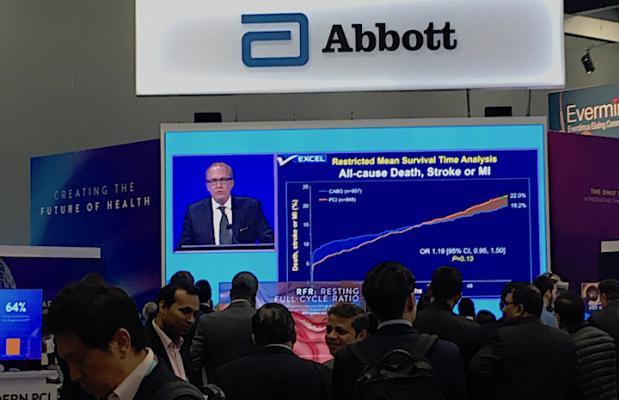
People watch the live presentation of the five-year EXCEL Trial data by Gregg Stone, M.D., in the Abbott booth at TCT 2019. Abbott makes the Xience stent used in the trial, which compared equally with long-term CABG surgical outcomes.
January 2, 2020 — In early December 2019, leaders of the European Association for Cardiothoracic Surgery (EACTS) withdrew their support for European practice guidelines that endorse the use of coronary stents in many patients with left main coronary artery disease. EACTS leadership said the reason was because the results of the EXCEL randomized clinical trial were misleading because of the definitions used for myocardial infarction (MI).[1]
The five-year data from the EXCEL Trial showed patients with left main coronary disease treated with percutaneous coronary intervention (PCI) using the Xience stent or coronary artery bypass graft surgery (CABG), had similar similar long-term, composite outcomes. The findings were reported at the 2019 Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium in September. Read more about the trial results.
However, there was some dispute from a few surgeons that the results actually showed surgery had better long term outcomes and claims that the definitions used in the study were chanbged to make stenting look more favorable.
The EACTS Council decided Dec. 7 to withdrew its support from the current recommendations on treatment of left main coronary artery disease (LMCAD) in the 2018 joint ESC-EACTS Myocardial Revascularization Guidelines. The society said this decision was based on a range of scientific, statistical and professional issues that had been raised. The Council also requested that ESC participate in a new joint task force to review the LMCAD recommendations in the guidelines.
EACTS said the protocol MI definition was based on the Society of Cardiovascular Angiography and Interventions (SCAI) definition of MI.[2] EACTS said this does not align with the Third Universal Definition of MI[3] developed collaboratively by the European Society of Cardiology (ESC), the American College of Cardiology (ACC), the American Heart Association (AHA) and World Health Foundation (WHO). These definitions differ in the recommended biomarker measurements and thresholds for adjudicating a periprocedural MI.
EACTS leaders further expressed concern that mortality rates were greater among stent-treated patients in EXCEL and suggested that the trial leadership was not forthcoming about this observation.
In a statement from the EXCEL Trial leadership, the MI definition was agreed to by all parties involved in the trial, including cardiac surgeons. Trial authors preferred the SCAI definition of MI because it was based on the best available evidence linking biomarker abnormalities to subsequent mortality in large clinical trials. They said the definition used also avoids ascertainment bias, and uses the same criteria for percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG) surgery.[4] Trial leaders also argued the SCAI definition has been used in multiple clinical trials because it avoids the pitfall of tabulating MI events that are small enough to have little clinical impact. Instead, the SCAI definition permits assessment of MI events that are likely to be clinically relevant.
EACTS claimed the MI definition used in the trial was changed, which the EXCEL investigators say is "absolutely incorrect." The trial leadership said the principal definition of MI never changed throughout the course of the trial.
Cumulative event curves for all-cause death for the two treatment groups in EXCEL were superimposable for the first 18 months after treatment, but separated from 18 to 36 months. Even though the difference was not statistically important at three years, it raised concerns that death rates would rise further for PCI-treated patients.[1] For this reason, the recent publication of five year follow-up for EXCEL patients in the New England Journal of Medicine was welcomed.[5] The paper shows that all-cause mortality remains higher for PCI-treated patients (13 percent versus 9.9 percent), but no difference in definite cardiovascular death was observed (5 percent versus 4.5 percent). The powered composite endpoint of death, stroke or MI was not different at three or five years of follow up.
EACTS stressed the all-cause mortality data from EXCEL was not strongly enough emphasized, but trial leaders said this was a secondary, underpowered endpoint. They said the modest difference noted between groups was not adjusted for multiplicity and is therefore statistically uncertain. EXCEL leaders said in addition, it has no biological basis given that the clinical events committee adjudicated the excess to be principally due to sepsis and cancer occurring years after randomization.
EXCEL authors cite a meta-analyses of 4,394 patients from four trials of drug-eluting stents vs. CABG (including EXCEL) show there is no difference in five-year mortality between PCI and surgery for left main disease. Even longer-term data (10-year follow-up from the SYNTAX trials) shows no difference in mortality. The distinction between all-cause mortality and cardiovascular mortality (which was very similar between PCI and CABG in EXCEL) was unfortunately not mentioned when this issue was discussed in a recent BBC interview with EACTS leadership.
SCAI said it respectfully disagrees with EACTS regarding EXCEL. In a statement, the society said while all-cause mortality is an important endpoint to follow, the EXCEL Trial was neither designed nor powered to assess differences in this endpoint. Lethal differences in treatment effectiveness would be expected to manifest as differences in cardiovascular death rates; while this was also an unpowered observation, the lack of any difference in definite cardiovascular death at five years is reassuring. SCAI said it endorses the guidelines in Europe and the United States that support use of coronary stents for treatment of left main coronary artery disease in appropriately selected patients.
Read the response from the EXCEL Investigators.
References:


 January 05, 2026
January 05, 2026 









