October 2, 2018 — Intravascular ultrasound (IVUS) guidance improved clinical outcomes over angiography guidance during drug-eluting stent (DES) implantation by lowering the rate of target vessel failure at one year in the ULTIMATE trial.
Findings from the all-comers trial were reported at the 30th annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium, Sept. 21-25 in San Diego, and published simultaneously in the Journal of the American College of Cardiology (JACC).1
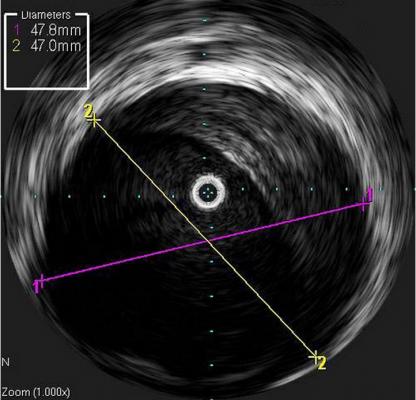
IVUS is an intravascular imaging modality that provides detailed anatomic information about reference vessel dimensions and lesion characteristics, including severity of diameter stenosis, lesion length and morphology (vulnerable plaque), which is less well-detected by coronary angiography. Whether the routine use of IVUS is associated with improved outcomes in allcomer patients is not known.
From August 2014 to May 2017, a total of 1,448 all-comer patients from eight centers in China who were undergoing DES implantation were randomly assigned (1:1) to either IVUS guidance (n=724) or angiography guidance (n=724). Multi-vessel disease was seen in 54.9 percent of patients. Mean lesion length was 34.5 mm, and 66.9 percent of lesions were classified as Type B2/C lesions. IVUS-guided procedures were longer in duration, and on a per-lesion basis used slightly greater stent diameters and stent lengths.
The primary endpoint was target vessel failure (TVF) at 12 months, defined as the composite of cardiac death, target vessel myocardial infarction (TVMI) and clinically driven target vessel revascularization (TVR). At 30-day follow up, primary and secondary endpoints were comparable between the two groups.
One year after PCI, a total of 60 (4.2 percent) TVFs occurred, with 21 (2.9 percent) in the IVUS group and 39 (5.4 percent) in the angiography group (HR 0.530; 95 percent CI: 0.312-0.901; p=0.019). In lesion-level analyses, the IVUS group had a lower rate of target lesion revascularization (TLR) compared with the angiography group (0.9 percent vs. 2.3 percent, p=0.02). Despite the use of IVUS, 53 percent of patients met prespecified optimal criteria for stent implantation; in this group, TVF was 1.6 percent, compared with 4.4 percent in patients who failed to achieve all optimal IVUS criteria (HR 0.349; 95 percent CI: 0.135- 0.898; p=0.029).
“The study demonstrated that IVUS-guided stent implantation significantly improved clinical outcomes in all-comers, particularly for patients who had an IVUS-defined optimal procedure, compared to angiography guidance,” said Junjie Zhang, M.D., vice director of the Cardiovascular Department at Nanjing First Hospital in Nanjing Medical University (Nanjing, China). “While previous studies and this trial have demonstrated the overall favorable effect of IVUS guidance for patients with particular lesion subsets, this study further reports that achievement of IVUSdefined optimal PCI improves clinical outcomes for all-comers.”
The ULTIMATE trial was funded by the National Natural Science Foundation of China and was jointly supported by Six Talent Peaks Project in Jiangsu Province, Nanjing Health and Family Planning Commission, Nanjing Health Youth Talent Training project, and Nanjing Municipal Commission of Science & Technology. Dr. Zhang has no conflicts of interest.
Click here to read more about late-breaking clinical trials at TCT 2018.
For more information: www.onlinejacc.org
Reference


 January 05, 2026
January 05, 2026 









