May 26, 2015 — St. Jude Medical Inc. announced preliminary results from the ILUMIEN I trial and final results from the ILUMIEN II clinical study. Taken together, the findings from both studies show that with resolution up to 10 times higher than intravascular ultrasound (IVUS), optical coherence tomography (OCT) imaging can help improve stent selection and deployment, better support clinical decision-making and improve patient outcomes.
Data from both studies were presented as late-breaking clinical trials at EuroPCR 2015, and further advance the use of OCT imaging alongside percutaneous coronary intervention (PCI).
During PCI procedures, physicians use diagnostic imaging to make decisions related to stent sizing and to assess how to best keep the artery expanded to restore blood flow to the heart. For patients, this visualization is important, as inappropriate stent sizing can induce trauma to surrounding vascular tissue, while under-expansion can lead to future clotting (thrombosis) or a recurrence of vessel narrowing (restenosis).
Now, data from the ILUMIEN I study has revealed OCT imaging conducted pre- and post-PCI influenced physician decision-making in 65 percent of patients and is associated with reduced rates of myocardial infarction (MI), commonly known as heart attacks. The ILUMIEN II study found that OCT guidance can yield a similar degree of stent expansion, or support full stent deployment, in comparison to IVUS. Stent expansion is viewed as an important predictor of adverse outcomes for patients undergoing PCI, such as blood clotting (thrombosis) or the recurrence of blood flow restriction (restenosis).
ILUMIEN I assessed 418 patients suffering stable or unstable angina or non-ST segment elevation myocardial infarction (NSTEMI). The study’s 12-month data shows:
- OCT guidance conducted either pre- or post-PCI altered physician decision-making in 65 percent of patients.
- Pre-PCI OCT altered treatment planning in 55 percent of patients and led to changes in decisions related to stent length and diameter.
- OCT imaging was associated with a reduction of in-hospital MI when used pre- and post-PCI to change the procedural strategy.
“Many physicians have long suspected that OCT’s higher resolution could support treatment planning and PCI procedural technique, and the ILUMIEN I study is another important step toward confirming OCT can contribute to the perfection of PCI,” said William Wijns, M.D., Ph.D., co-director of the Cardiovascular Centre in Aalst, Belgium.
The ILUMIEN II study was designed to determine whether OCT guidance results in a comparable degree of stent expansion as IVUS imaging. After an analysis of OCT-guided stenting or IVUS-guided stenting in 940 patients from the ILUMIEN I and ADAPT-DES studies, the degree of stent expansion was found to be comparable between OCT and IVUS imaging. The study’s data shows OCT and IVUS guidance were also associated with comparable rates of major stent malapposition, tissue protrusion and stent edge dissection.
“The results of ILUMIEN II address long-standing questions regarding the ability of OCT guidance to achieve comparable stent expansion, more precise measurements and a greater level of vascular visualization than first generation imaging tools such as IVUS,” said Gregg W. Stone, M.D., professor of medicine, Columbia University Medical Center and Study Chairman of Ilumien II. “Now, the results of angiography-guided, IVUS-guided and OCT-guided stent implantation are currently being evaluated in the prospective, multicenter ILUMIEN III: OPTIMIZE PCI randomized trial.”
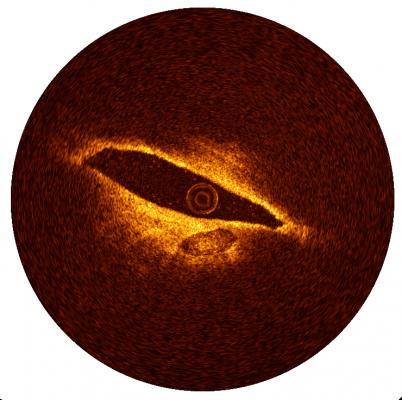
St. Jude Medical’s OCT technology is an intravascular imaging tool that uses light to provide anatomical images of disease morphology and automated measurements. With OCT technology, physicians can visualize and measure important vessel characteristics that are otherwise not visible or difficult to assess with the older imaging technology. As a result, OCT can provide automated, highly accurate measurements that can help guide stent selection and deployment and assess stent placement to help ensure successful procedures. This can potentially minimize the need for repeat revascularization.
For more information: www.sjm.com


 January 05, 2026
January 05, 2026 









