March 6, 2014 — Despite good immediate results, in up to 40 percent of patients, obstructed arteries in the leg treated with a stent will again become blocked. This in-stent restenosis is typically treated with balloon angioplasty to clear the artery. The addition of drug-eluting balloons is showing improved outcomes for restenosis and could become the treatment of choice for femoropopliteal in-stent restenosis.
The Journal of Endovascular Therapy offers results of a prospective study seeking to establish the rate of one-year restenosis in diabetic patients with femoropopliteal in-stent restenosis who underwent treatment with drug-eluting balloon angioplasty. The study is known as Drug-Eluting Balloon in Peripheral Intervention for In-Stent Restenosis, or DEBATE–ISR.
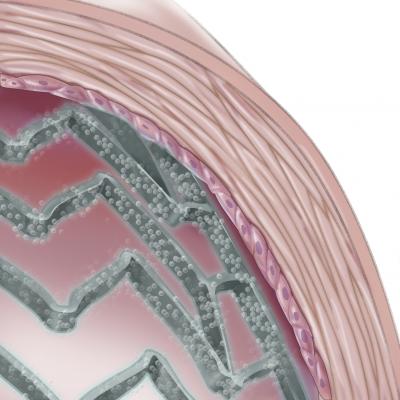
Conventional treatment of restenosis in femoral and popliteal arteries relies on repeat high-pressure dilation with balloons, which has a high rate of recurrent restenosis. The drug-eluting balloon delivers paclitaxel as it expands within the stent. Paclitaxel is an antiproliferative drug that inhibits microtube formation and subsequent ingrowth of smooth muscle cells.
In this study, 44 diabetic patients were treated for femoropopliteal in-stent restenosis with the drug-eluting balloon. After one year, their recurrent restenosis rate was compared with that of a control group—42 diabetic patients previously treated with standard balloon angioplasty for in-stent restenosis.
A significant reduction in restenosis was achieved. Study results show that only 19.5 percent of patients treated with the drug-eluting balloon experienced recurrent restenosis after one year, whereas those treated with standard balloon angioplasty had a 71.8 percent rate of recurrence. Additionally, only 13.6 percent of patients in the drug-eluting balloon treatment group underwent target lesion revascularization compared with 31 percent of those in the control group.
These results offer reassurance to physicians about the safety of this procedure. They also put forward a promising alternative to the other restenosis technologies and strategies that have shown mixed outcomes.
An accompanying commentary notes that while further studies are needed, these results are encouraging. The authors point out the limitations of the study, including the absence of randomization and use of the historical control group. However, they state that the results for these diabetic patients “are particularly impressive in light of the high-risk patient population being treated.”
For more information: jevt.org


 January 05, 2026
January 05, 2026 









