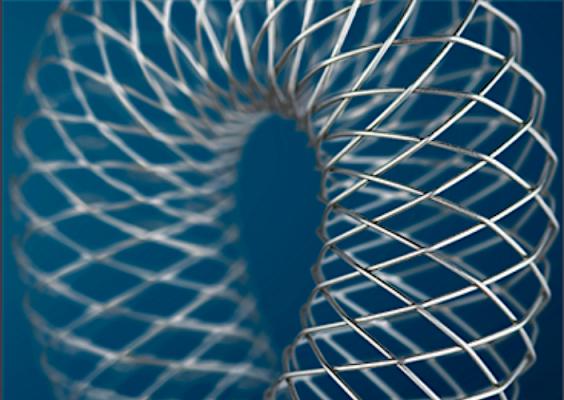
The repuncturable Supera vascular mimetic peripheral stent system from Abbott Vascular was shown to manage bulky, heavily calcified CFA disease due to its extreme crush resistance in the VMI-CFA study.
November 11, 2019 — Although common femoral artery (CFA) endarterectomy is still considered the gold standard treatment for patients with CFA stenosis, 12-month follow-up results of the VMI-CFA study showed that endovascular stent repair is a safe and effective alternative. The results were presented at the 2019 Vascular Interventional Advances (VIVA) annual meeting.
The repuncturable Supera vascular mimetic peripheral stent system from Abbott Vascular was shown to manage bulky, heavily calcified CFA disease due to its extreme crush resistance, explained presenter Koen Deloose, M.D., head of vascular surgery, AZ Sint-Blasius Hospital, Dendermonde, Belgium. These two-year data confirm that CFA disease can be treated endovascularly with the Supera stent with great outcomes and a very good safety profile. He said a head-to-head randomized controlled trial of Supera vs. endarterectomy (SUPERSURG RCT) will be launched in 2020 to further clarify the CFA treatment discussion.
The multicenter, prospective, single-arm VMI-CFA trial evaluated the outcomes of treatment of symptomatic (Rutherford class 2–4) CFA stenotic or occlusive lesions with the Supera stent in 100 patients. All patients had de novo lesions (> 50% stenosis). The primary efficacy endpoint was core lab–assessed duplex ultrasound primary patency at 12 months, and the primary safety endpoint was the absence of peri-procedural adverse events up to 30 days post-procedure. The cumulative primary patency rates up to 365 and 395 days were 95.2 and 92.8%, respectively. The cumulative freedom from target lesion revascularization (TLR) rate was 97.8%. No procedure- or device-related adverse events were reported.
To investigate the longer-term durability of the endovascular approach, the 24-month VMI-CFA study results were prospectively analyzed. No new loss of primary patency or TLR was reported, resulting in a cumulative primary patency rate of 92.8% and a freedom from TLR rate of 97.8% at 730 days. The cumulative survival rate was 85.5%. The tremendous shift from Rutherford class 3-4 toward Rutherford class 0-1 was sustained at two years.
Find information on all the VIVA 2019 Late-breaking Clinical Trials


 January 05, 2026
January 05, 2026 









