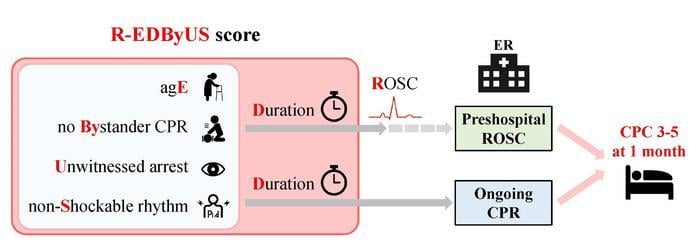
R-EDByUS score features variables using only prehospital resuscitation data. Image courtesy of Takenobu Shimada, Osaka Metropolitan University (CC BY 4.0, https://creativecommons.org/licenses/by/4.0/)
July 29, 2024 — When it comes to treating cardiac arrest, acting quickly can mean the difference between life and death.
Researchers from Osaka Metropolitan University have developed a new scoring model, using only prehospital resuscitation data, that accurately predicts neurological outcomes of patients with out-of-hospital cardiac arrest (OHCA). This model potentially allows healthcare providers to make quick and accurate decisions upon the patient’s arrival at the hospital, ultimately improving patient care and resource allocation. Their findings were published in Resuscitation on May 31.
Cardiac arrest can lead to death within minutes. OHCA is not uncommon and often results in low survival rates. In Japan, over 100,000 patients experience OHCA annually, with less than 10% returning to normal life.
Rapid and accurate neurological prediction calculations are critical in OHAC cases. Effective prediction models can save lives, reduce suffering, and cut down on unnecessary costs associated with futile resuscitation efforts.
“Current prognosis prediction models require complex calculations and blood test data, making them impractical for rapid use immediately after patient transport,” said Takenobu Shimada, a medical lecturer at Osaka Metropolitan University’s Graduate School of Medicine and lead author of the study.
The research team addressed this gap by constructing a scoring model that uses readily available prehospital data to predict unfavorable neurological outcomes. Analyzing data from the All-Japan Utstein Registry, they examined information collected between 2005 and 2019 on prehospital resuscitation and neurological recovery one month post-arrest for 942,891 adults with presumed cardiac-origin OHCA. Adverse outcomes include severe disability, vegetative state, or death.
Named the “R-EDByUS score,” the developed model is derived from the initials of its five variables: age, duration to return of spontaneous circulation (ROSC) or time to hospital arrival, absence of bystander CPR, whether the arrest was witnessed and, finally, initial heart rhythm (shockable versus non-shockable).
Patients were divided into two groups based on whether they achieved ROSC before hospital arrival or were still undergoing CPR upon arrival. The researchers developed detailed regression-based and simplified models to calculate R-EDByUS scores for each group.
The results demonstrated that the R-EDByUS scores predicted neurological outcomes with high precision, achieving C-statistics values of approximately 0.85 for both groups. C-statistics measure the predictive accuracy of a model, ranging from 0.5 (no predictive power) to 1.0 (perfect accuracy), with higher values indicating superior performance.
“The R-EDByUS score enables high-precision prognosis prediction immediately upon hospital arrival, and its application via smartphone or tablet makes it suitable for everyday clinical use,” Shimada said.
This scoring model is expected to become a valuable tool for healthcare providers, aiding in the prompt assessment and management of patients undergoing resuscitation.
“In emergency care for OHCA, invasive procedures, such as mechanical circulatory support, can be lifesaving but are also highly burdensome,” Shimada said. “Our predictive model helps identify patients who are likely to benefit from intensive care while reducing unnecessary burdens on those with poor predicted outcomes.”
For more information: www.omu.ac.jp/en/


 January 05, 2026
January 05, 2026 









