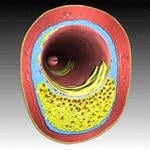
An example of vulnerable plaque.
October 8, 2009 – The primary results from its groundbreaking PROSPECT (Providing Regional Observations to Study Predictors of Events in the Coronary Tree) clinical trial were released at TCT 2009 in September, which shows promise in identifying and predicting how vulnerable plaque might progress to a cardiac event.
The Abbott-sponsored trial is the first prospective natural history study to examine the role of vulnerable plaque using intravascular imaging technology to correlate plaque characteristics, patient risk factors and biomarker measurements with subsequent heart attacks and other cardiac events, potentially paving the way for physicians to identify and treat at-risk patients before a heart attack occurs. PROSPECT enrolled 700 patients from 40 clinical centers across the United States and Europe. All patients received PCI for acute coronary syndrome (ACS), which included unstable angina, NSTEMI or STEMI. Patient follow up continued for three years. Abbott sponsored the study and VH IVUS imaging technology was provided by Volcano Corporation.
Results were presented during a late-breaking clinical trials session by Gregg W. Stone, M.D., professor of medicine at Columbia University Medical Center, during the 2009 Transcatheter Cardiovascular Therapeutics (TCT) annual meeting. "We know that certain vulnerable plaques lead to sudden cardiac death, but until now, our understanding of how these plaques progress has been extremely limited," said Dr. Stone. "PROSPECT has provided fundamental insights into our understanding of atherosclerosis. Conventional wisdom has been that if we could identify vulnerable plaques, we would be able to determine who might be at risk for a serious cardiac event and treat them prophylactically."
Vulnerable plaques are inflamed, lipid-rich lesions that form in the walls of the arteries and usually have thin, fibrous caps. The relationship between vulnerable plaque ruptures and sudden cardiac death is well known, but until the PROSPECT study, no systematic effort had been made to prospectively understand the event rate associated with progression of vulnerable plaque. Unlike hardened plaque, vulnerable plaques are often not visible with angiography and do not actually block blood flow in coronary arteries unless their rupture results in a clot.
Among the findings of the 700-patient study, researchers were able to identify the common characteristics of lesions that put patients at highest risk for future cardiac events by using advanced imaging called virtual histology intravascular ultrasound (VH IVUS) and standard angiography. Going forward, investigators will now have access to more than 40,000 datapoints derived from 150 variables within each of the patients, far beyond the level of assessment of previous interventional studies.
"While the prognosis of patients with acute coronary syndromes undergoing successful stenting and treated with contemporary medical therapy is favorable, we are now able to identify those lesion types with a significantly increased likelihood of causing future cardiovascular events," Stone said.
The PROSPECT study recruited patients who were in need of a PCI (percutaneous coronary intervention) to treat a heart attack or threatened heart attack. Patients consented to collection of additional data as follow-up to their procedure, including VH IVUS imaging and standard angiography. PROSPECT collected data about characteristics of vulnerable plaque lesions that were present but not causing symptoms at the time of the procedure. The goal was to correlate lesion characteristics, patient risk factors and biomarker measurements with subsequent heart attacks and other cardiac events, potentially paving the way for physicians to identify and treat at-risk patients before a heart attack occurs.
In the study, approximately 20 percent of the patient population experienced a major adverse cardiac event (cardiac death, cardiac arrest or heart attack) within three years of enrollment. Half of these events can be attributed to the original "culprit" lesions (those treated with PCI) and half to previously untreated, "nonculprit" lesions of the three-vessel coronary tree. Half of the patients treated for non-culprit events exemplified the classic notion of vulnerable plaque.
The event rate, particularly that attributed to vulnerable plaques specifically, was lower than expected. Further, patients who experienced "nonculprit" events in the years following PCI were more likely to present with progressive or unstable angina, and rarely with cardiac death, arrest or MI. Imaging of the lesions that did progress to events suggests that vulnerable plaque lesions with a large plaque burden and large necrotic core without a visible cap were at especially high risk for future adverse cardiovascular events.


 January 05, 2026
January 05, 2026 









