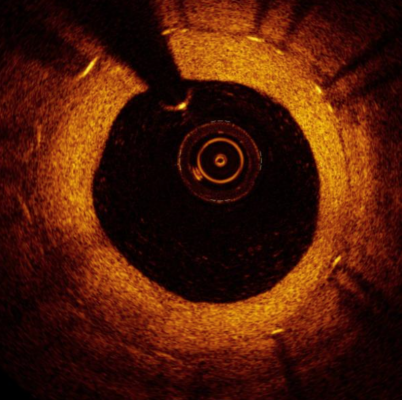
An OCT intracoronary image showing instent restenosis. The white spots in the vessel wall casting shadows are the stent struts. OCT image data might be used in the future to assess FFR to determine the severity of lesions and determine if they need to be stented.
May 15, 2020 – A late-breaking study aimed to evaluate whether optical coherence tomography (OCT) can predict fractional flow reserve (FFR) values and assess if OCT parameters may predict clinical outcome in patients with negative FFR. The study was presented at the Society for Cardiovascular Angiography and Interventions (SCAI) 2020 Scientific Sessions Virtual Conference.
OCT imaging offers high-resolution intracoronary imaging technique used to characterize plaque morphology and to guide optimization of percutaneous coronary intervention (PCI). It also might provide some insights into the physiological, functional significance of a stenosis.
“The idea of predicting hemodynamic relevance of coronary lesions from imaging is extremely appealing. In this collaborative study we sought to investigate if OCT parameters may help predicting the presence of hemodynamically significant stenoses among angiographically-intermediate coronary lesions (AICL)," said Rocco Vergallo, M.D., Ph.D., Fondazione Policlinico Universitario Agostino Gemelli, Rome, Italy. “We put together data collected from different studies so that we have been able to analyze individual data of about 500 patients.”
The research team, under the leadership of Francesco Burzotta, M.D., lead investigator, Institute of Cardiology, Catholic University of the Sacred Heart, Rome, Italy, designed a multicenter, international, study using individual patient's level data pooled analysis. Stable or unstable patients who underwent both FFR and OCT of the same coronary lesion were enrolled. Primary outcome measures were OCT parameters predicting an FFR <0.80, including mean lumen area (MLA), percentage area stenosis (%AS), and presence of plaque thrombus/rupture. =
Secondary outcome was the incidence of major adverse cardiac events (MACE) in patients not undergoing revascularization based on negative FFR (≥0.80). MACEs were defined as the composite of cardiac death, spontaneous myocardial infarction (MI) and target lesion revascularization.
A total of 502 coronary lesions in 489 patients were included. A significant correlation was observed between OCT-MLA and FFR values (R=0.525, p<0.001), and between OCT-%AS and FFR values (R=-0.482, p<0.001), while plaque thrombus/rupture did not differ significantly. At ROC analysis, an OCT-MLA <2.0 mm2 showed a good discriminative power to predict an FFR<0.80 (AUC 0.80), as well as an OCT %AS >73% (AUC 0.73). When considering proximal coronary segments only, the best OCT cut-off values predicting an FFR<0.80 were MLA <3.1 mm2 (AUC 0.82), and %AS >61% (AUC 0.84). Among 105 patients who had not undergone revascularization based on negative FFR and had completed the clinical follow up, 11 (10.5%) had MACE. Median follow-up time was 6 years (IQR: 2.3-8.3). Patients with MLA <2 mm2 showed a non-significantly higher incidence of MACE than those with MLA ≥2 mm2 (16.7% vs. 9.2%, p=0.139).
“These findings are important because they may allow interventional cardiologists to gather both data on plaque morphology/lumen dimension and indirect information on the functional significance of a stenosis by using an imaging catheter only, without the need for an additional pressure wire,” Vergallo continued. “This would, in turn, reduce both patient risk and healthcare expenses.”
For more information: www.scai.org


 January 05, 2026
January 05, 2026 









