Implantation of pacemakers, ICDs and the related cardiac leads opens patients to infection risk.
May 10, 2018 – A new study is the first to test the clinical effectiveness of incremental peri-operative antibiotics as a method to reduce potential infection of cardiac implantable electronic devices (CIEDs). The trial compared the novel peri-operative antibiotics strategy to the conventional treatment of pre-procedural cefazolin, a common antibiotic. The Prevention of Arrhythmia Device Infection Trial (PADIT) study included 19,603 patients from 28 centers and is the first time a randomized cluster cross-over design has been used in CIED patients. The results of the study were presented at Heart Rhythm 2018, the Heart Rhythm Society’s 39th Annual Scientific Sessions.
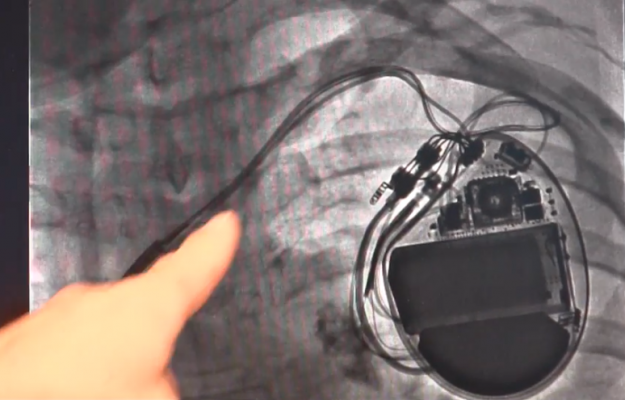
CIED devices, like pacemakers and implantable cardioverter-defibrillators, are a common treatment option for patients suffering from cardiac arrhythmias. Today, about 400,000 devices are implanted annually, and more than 3 million Americans have CIEDs.[1] Infection of implanted medical devices can have serious consequences for patients. Currently, antibiotics are often administered before the procedure as a precaution but are not guaranteed to protect against common pathogens found in device infections. This is the first study to evaluate the effectiveness of incremental peri-operative antibiotics to reduce device infection.
Twenty-eight centers were randomized to use either conventional or incremental antibiotic treatment in all patients at the time of device implant over four six-month periods. The trial included 19,603 patients, of whom 12,842 were high-risk. The mean patient age was 72 ± 13.1 years old and 40 percent had a history of heart failure. Conventional treatment was pre-procedural cefazolin infusion. Incremental treatment was pre-procedural cefazolin plus vancomycin, intra-procedural bacitracin pocket wash and two-day post-procedural oral cephalexin. The primary outcome was one-year hospitalization for device infection analyzed by hierarchical logistic regression modeling, adjusting for random cluster and cluster-period effects.
Infection occurred in 99 patients (1.03 percent) receiving conventional treatment, and in 78 (0.78 percent) receiving incremental treatment. In higher risk patients, hospitalization for infection occurred in 77 (1.23 percent) patients receiving conventional antibiotics and in 66 (1.01 percent) receiving incremental antibiotic. The observed difference in infection rates was not statistically significant but was consistent with a modest benefit from incremental antibiotics.
“Infections of these devices, while not very common, can have a long-lasting and devastating impact on patients. It’s really important that we explore robust measures to prevent infections from occurring,” said lead author Andrew Krahn, M.D., head of the division of cardiology and professor of medicine at the University of British Columbia. “Our results show that incremental antibiotics strategy can have a modest, positive effect when the infection rate is low. We hope that our study will help clinicians identify patients that may benefit from this treatment option and utilize a targeted, high intensive antibiotic strategy to reduce and prevent infections.”
The authors note that this topic will continue to be investigated with another clinical study “World-wide Randomized Antibiotic Envelope Infection Prevention Trial (WRAP-IT),” which examines an antibiotic envelope device that is put into the pocket where the surgery is performed to assess the efficacy of reducing infections. Results of this study are expected to be published in 2019.
Find links to all the Heart Rhythm 2018 Late-breaking Studies
Reference:
#HRS2018


 January 05, 2026
January 05, 2026 









