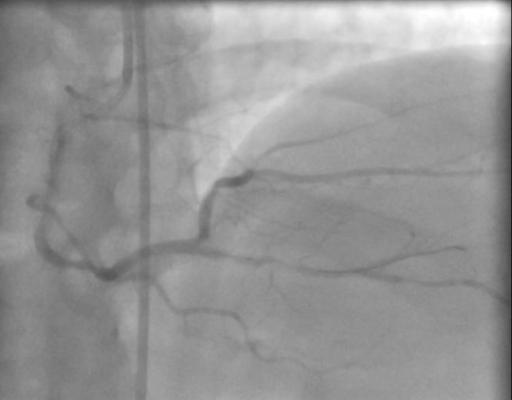
September 25, 2019 — Ten-year survival rates are similar for bypass surgery and coronary stenting with drug-eluting stents in randomized patients with de novo three-vessel and left main coronary artery disease, according to new research. The late-breaking results from the SYNTAX Extended Survival study were presented in a Hot Line Session at the European Society of Cardiology (ESC) Congress 2019, Aug. 31-Sept. 4 in Paris, France, together with the World Congress of Cardiology and published in The Lancet.[1]
Prespecified subgroup analyses showed that surgery provided a survival benefit in patients with three-vessel disease and more complex coronary artery disease, while no treatment differences were found in patients with left main disease.
Ischemic heart disease is the top cause of death globally. Percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) are options for patients requiring revascularization. European guidelines advise discussing these patients in a multidisciplinary heart team. [2]
Individual randomized trials comparing PCI with drug-eluting stents and CABG have not shown a survival benefit for either therapy at mid-term follow-up (e.g. up to five years). The SYNTAX trial was the first large-scale multicenter, randomized study in patients with de novo three-vessel and left main coronary artery disease that underwent PCI with drug-eluting stents or CABG. When clinical equipoise between PCI and CABG was presumed by the heart team, 1,800 patients were randomly assigned to PCI with paclitaxel-eluting stents (n=903) or CABG (n=897). Survival curves started to diverge after one-year follow-up[3] and continued to diverge up to five years, but without reaching statistical significance.[4]
The SYNTAX Extended Survival (SYNTAXES) study examined 10-year all-cause death rates in patients with de novo three-vessel and left main coronary artery disease randomized to PCI with drug-eluting stents or CABG in the SYNTAX trial. All 85 SYNTAX sites from 18 North American and European countries were contacted to provide survival data, which was obtained from healthcare records and national death registries. Completeness of follow-up was achieved in 94 percent of patients and was well-balanced between the CABG and PCI arms.
At 10-year follow-up, there was no survival difference between PCI with drug-eluting stents and CABG in the overall cohort of patients. There were 244 deaths after PCI and 211 after CABG (hazard ratio [HR] 1.17; 95 percent confidence interval [CI] 0.97–1.41; p=0.092).
When analyses were conducted according to prespecified subgroups, CABG provided a 10-year survival benefit over PCI in patients with three-vessel disease (151 deaths after PCI versus 113 after CABG; HR 1.41; 95 percent CI 1.10–1.80; p=0.006). CABG also provided a survival benefit in patients with increasingly complex coronary artery disease (defined by higher SYNTAX scores) – this was observed in the overall cohort and in those with three-vessel disease. In the subgroup of patients with left main coronary artery disease, no survival differences existed between PCI and CABG (93 patients died after PCI versus 98 after CABG; HR 0.90; 95 percent CI 0.68–1.20; p=0.47). This resulted in a treatment-by-subgroup interaction according to the presence or absence of left main coronary artery disease (p for interaction=0.019). Furthermore, CABG and PCI resulted in comparable 10-year survival in patients with and without diabetes.
First author Daniel Thuijs, M.D., of the Erasmus University Medical Centre, Rotterdam, the Netherlands said, “The SYNTAX Extended Survival study presents robust, clinically relevant and complete 10-year randomized survival data and can aid a multidisciplinary heart team discussion in the process of deciding on the optimal treatment strategy for a patient with coronary artery disease requiring revascularization.”
For more information: www.escardio.org
References
1. Thuijs D.J.F.M., Kappetein A.P., Serruys P.W., et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. The Lancet, published online Sept. 2, 2019. https://doi.org/10.1016/S0140-6736(19)31997-X
2. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165. doi:10.1093/eurheartj/ehy394.
3. Serruys P.W., Morice M.C., Kappetein A.P., et al. Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease. N Engl J Med. 2009;360:961–972.
4. Mohr F.W., Morice M.C., Kappetein A.P., et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381:629–638. doi: 10.1016/S0140-6736(13)60141-5.


 January 14, 2025
January 14, 2025