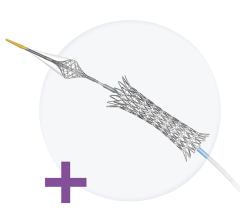
The CoStar drug-eluting stent by Conor MedSystems features tiny reservoirs that are filled with drugs and polymer.
Author’s Note: For this inaugural article I begin with an insider’s look on the “health” of drug-eluting stents and what lies ahead for this much-debated device.
I also introduce two companies that were both started in Israel. In December I was invited to attend the Innovations in Cardiovascular Interventions (ICI) meeting in Tel Aviv. The meeting is held annually and is co-organized in partnership with the Israel Heart Society and the Cardiovascular Research Foundation in New York. I had the opportunity to meet with several company leaders and to learn about some very exciting and innovative technologies.
Drug-Eluting Stents: Current Status, Future Forecast
World-renowned interventional cardiologist Patrick Serruys, M.D. (Erasmus Medical Center, Rotterdam, the Netherlands) was able to take a few minutes to share his thoughts regarding the current health and future of DES during the ICI meeting.
2006: A Special Year For DES?
Dr. Serruys said 2006 was a “special year” for DES because it was “the year of the European Cardiology Society fire storm.” He noted that the hype surrounding stent thrombosis all started with the ESC when it drew “strange” connections between late stent thrombosis, death, myocardial infarction and noncardiac mortality.
The “Year of the DES” was culminated with a two-day FDA advisory panel that took place in December where a panel of physician experts, which included Dr. Serruys, discussed safety issues associated with DES use. The panel concluded that: (1) Although the risk of stent thrombosis was real, when used as indicated, no significant increases in death or MI were observed; and (2) The panel advised using caution when considering the off-label use of DES.
Dr. Serruys said there are three ways to potentially address the DES-stent thrombosis problem: (1) Initiate lengthy, long-term pharmacological safety trials of antiplatelet drugs; (2) Conduct more head-to-head DES safety studies, such as the Medtronic PROTECT trial that will compare the frequency of stent thrombosis between Medtronic's Endeavor stent and Cordis' Cypher stent; or (3) Take an alternative, yet innovative, approach by examining what other technologies exist that might help resolve the problem.
“My preferred approach is to go with 'innovation' and to see if that can resolve the issue,” said Dr. Serruys.
Are Polymer Coatings the Problem?
Dr. Serruys ventured that one way of mitigating stent thrombosis is by reducing or eliminating the amount of durable polymer coating that is applied to DES.
“The first step,” he said, “is to try to reduce the amount of durable coating applied to DES because [it is] causing hypersensitivity, [it is] thrombogenic, and [it is] fragile and can crack during [stent deployment].”
He believes that advances in biomaterial coatings, such as hydroxapatite and nanocarbons, might reduce the overall thrombogenecity and in some cases, the hypersensitivity patients have to current DES. He also noted that coating stents ablumenally — coating the side of the stent that comes in contact with the vessel wall — might help too.
Then there are the re-absorbable polymers, which Dr. Serruys says disappear completely once the drug is eluted from the stent.
“There are several of these stents in development in Europe with either biodegradable polymers or bioresorbable coatings, such as those being produced by Biosensors and Conor Medsystems, which might completely take care of the stent thrombosis issue,” he said.
Another option, according to Dr. Serruys, is to examine the potential application of metal-free, bioresorbable stents.
“Next is trying to eliminate the metal altogether, so that the 'backbone' disappears,” stated Dr. Serruys. However, he believes metal-free bioresorbable stent technology is “next, next, next- generation DES technology.”
Are Drugs The Issue?
“We need to reduce the amount of cytostatic and cytotoxic drugs that are applied to DES,” Dr. Serruys said.
He pointed out that sirolimus and paclitaxel are drugs that inhibit the cell cycle, and both, he says, interfere with endothelialization. He believes more focus should be placed on testing drugs that can address acute issues associated with stent implantation, such as stent thrombosis and inflammation, and that less emphasis needs to be placed on testing drugs that have an affect on smooth muscle cell (SMC) proliferation and proteoglycan production (PP).
“By killing smooth muscle cells you eliminate two phases of restenosis; however, you are still left with the issues of thrombosis and inflammation,” he explained. “But it also makes sense to work on [controlling thrombosis and inflammation], where the amount of either cytostatic or cytotoxic drug that is needed to control [SMC proliferation and PP] can be reduced.”
Dr. Serruys noted that a few companies are currently experimenting with alternative drugs, such as pimecrolimus and tacrolimus, which affect the cell mechanism in a different way. For example, pimecrolimus, currently being evaluated by Conor Medsystems, is an anti-inflammatory drug that blocks cytokines and acts on the “Go1 Phase” of the cell cycle. That is the phase prior to the cell entering its reproduction cycle.
“These types of drugs deactivate the cell without killing it,” said Dr. Serruys.
What About Drug Delivery?
Dr. Serruys believes there are several advantages to having built-in reservoirs or wells designed into stents for the delivery of drugs.
“There are two big advantages of reservoirs: (1) you are not obligated to circumferentially coat the stent, and (2) multiple drugs can be used. Take Conor's CoStar stent for example. Because its stent has adjacent wells, the wells can hold different drugs.”
He says this takes drug delivery to the next level because it creates a dual-elution stent. The dual-elution stent becomes very beneficial, he believes, particularly if a stent manufacturer can couple two synergistic drugs, such as paclitaxel and pimecrolimus. Even though a drug like pimecrolimus is not as effective at controlling SMC proliferation, it is much less harmful to endothelial cell production.
“In that case, you can start reducing the cytotoxicity of [paclitaxel] because less of the drug is needed,” he said. “By coupling synergistic drugs together you are creating a gradient of safety.”
Dr. Serruys said that Conor’s dual paclitaxel-pimecrolimus stent (called SymBio) has performed very well in animals, and now the company is evaluating the dual elution stent in humans.
What's Next?
In summary, Dr. Serruys said bioresorbable and ablumenal coatings, mechanical reservoirs, dual elution-profiled stents and drugs that act on inflammatory response rather than on cell proliferation are what the market can expect in the next iterations of DES.
“We are really still at the beginning of the drug- eluting stent era,” he noted.
And he anticipates a time when physicians have the perfect DES: one that is completely absorbable, lumenally coated (with endothelia progenator cells) and capable of delivering multiple drugs.
New Product From Rcadia Will Enhance CTA
Imagine being able to rule out coronary artery disease (CAD) as the culprit for acute chest pain and getting the results in a matter of minutes, without having to go to the cath lab for diagnosis. Increasingly, multidimensional computed tomography (MDCT) is being offered as a diagnostic tool in emergency departments across the U.S. and may eventually become the diagnostic modality of choice used to triage patients who present to the ER experiencing chest pains.
“When a patient arrives to the emergency department complaining of chest pain, ER staff will check for three things: a cardiac event, a pulmonary embolism and an aortic dissection,” said Hillel Bachrach, chairman of Rcadia Medical Imaging Technology (Haifa, Israel) after his presentation at the ICI meeting called “Rcadia — The Next Frontier in MDCT Cardiac Imaging.”
Bachrach said current CT systems are incapable of performing a “triple rule-out,” which is ER jargon for ruling out whether chest pain is caused by a cardiac event, a pulmonary embolism or an aortic dissection in a single CT pass/scan.
“What companies like GE Healthcare have focused on is honing their systems to rule out CAD as the culprit for acute chest pain by using CTA,” he said..
With the “Click” of a Mouse
The COR Analyzer family of CT angiography (CTA) applications from Rcadia, which is financed by a U.S. equity investment firm, will do just that — provide ER staff a definitive answer as to whether acute chest pain is caused by CAD or something else.
“Today's CT systems are more readily available to ER personnel,” indicated Bachrach. For example, he pointed to Massachusetts General in Boston where the CTA system is located one floor above the ER, and to Beth Israel Hospital, also in Boston, where two CTA systems are located in the emergency department.
“If you really want CTA to provide the most value at the most critical time, the physician in the emergency department needs to be able to quickly rule out CAD as the culprit for chest pain,” said Bachrach.
He indicated that what is truly unique about Rcadia's CTA image processing software is its ability to tell the physician whether the chest pain the patient is experiencing is actually caused by heart attack.
“COR Analyzer can accomplish this task with a single click of a [computer] mouse.”
Rcadia's computer-aided diagnostic software uses proprietary image processing algorithms to analyze cardiac CTA cases, known as “studies,” to determine whether the chest pain was caused by the presence of CAD. Rcadia's software triage process is based on automatic reconstruction and analysis of the CT images.
Bachrach attributed the uniqueness of Rcadia's CTA software to its ability to quickly process CTA images slice by slice and to rule out CAD. He said Rcadia set the bar high when they started testing the software.
“We thought we could achieve 96 or 97 percent negative predictive value, but the software actually correctly ruled out CAD in 100 percent of the cases in our first 20 patients,” he said. “At first we attributed our initial success to luck, but now, with 96 patients completed and having successfully ruled out CAD in all 96, and in 99 percent of the arteries we examined, our success can no longer be attributed to luck.”
“CT angiography is being rapidly adopted to triage patients in America's ERs,” said George Holland, M.D. (Lahey Clinic, Boston, MA), a physician with ties to Rcadia,. “Rcadia's COR Analyzer software can quickly identify and exclude CAD with a high degree of accuracy and thus, it streamlines patient care and prevents unnecessary delays in diagnosis and care.”
Dr. Holland stated that the real benefit of Rcadia's software is the High Negative Predictive Value (or High NPV) of screening out “false positives,” by identifying those patients with “true” negative tests, and accordingly, that do not have CAD.
More than 5 million patients in the U.S. present to the ER each year with acute chest pain, according to Bachrach, and current diagnostic modalities do not effectively triage patients with acute chest pain with normal cardiac enzyme levels and ECGs. Deciding on the appropriate treatment for these patients causes a variety of clinical and work-flow related issues in the ER. On one hand, missing clinically significant CAD can lead to morbidity; on the other hand, misdiagnosing insignificant CAD can lead to further, unnecessary cardiac evaluations.
Blazing Its Own CorPath
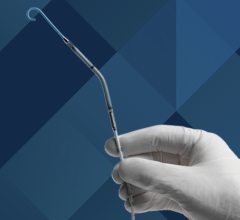
The field of angioplasty is evolving rapidly. The speed at which new technologies are emerging is astonishing. One technology in particular that stands out is the CorPath Remote Controlled Angioplasty System from Corindus, Inc.
The CorPath system allows an operator to safely perform PCI outside the cath lab's direct radiation field. Tal Wenderow, Corindus' CEO, told Diagnostic & Invasive Cardiology following his ICI meeting presentation that “CorPath will make PCI much safer and more reliable, particularly during long, drawn-out cases, because the human factor of directly manipulating guidewires and catheters tableside is eliminated.”
Several studies have shown that over time, endovascular specialists can develop lower back and joint problems from standing long hours and regularly wearing leaded protective gear. However, with CorPath, an electro-mechanical box called the “Bedside Unit” is attached to the cath lab table and tethered to the system's remote workstation in the cath lab. From the remote work station, the operator is protected from X-ray radiation due to the workstation's protective shield. In most cases, the operator doesn't have to wear heavy leaded garments. More importantly, noted Wenderow, “the operator retains full control over the entire procedure from the workstation, advancing and positioning instruments, deploying stents, and operating the C-Arm. Furthermore, the operator can perform the entire procedure while comfortably seated.”
Route 510(k)
Corindus completed its animal and first-in-man (FIM) trials approximately a year ago, and is now working with the FDA to finalize its Investigational Device Exemption (IDE) to start human clinical trials in the U.S. The CORRECT Trial, (Coronary Remote Control Catheterization), will be carried out at five sites within the Boston-Washington, D.C. corridor, and will be lead by Dr. Ron Waksman of Washington Heart Center (Washington, D.C.)
“We've already recruited our sites and have begun training the investigators on the CorPath system at our office in Auburndale, MA,” said Wenderow.
The CorPath will be a 510(k) system and will use Stereotaxis' Magnetic Navigation System as the predicated device. Wenderow anticipates receiving FDA clearance in late 2007 and emphasizes that CorPath will be the only commercially available remote control system with an indication for PCI.
Tools of the Trade
Once cleared, the system will use off-the-shelf guidewires and catheters.
“One of CorPath's distinct features is its compatibility with conventional 0.014-inch angioplasty instruments. This makes the CorPath extremely versatile and very user friendly.” Wenderow noted that other “remote navigation systems” are not so flexible and require specialty catheters and guidewires, such as Stereotaxis' magnetic guidewires that are needed in order to use that system.
“This makes CorPath more cost effective, since physicians can continue to use their preferred instruments,” he said. “The only disposable items on our system are the Bedside Unit manipulators. These are the only single-use devices.”
The replacement cost for a set of Bed Unit manipulators will be in the hundreds of dollars, giving cath labs a significant cost savings over the $1,000 price necessary to replace used magnetic guidewires.
Another distinct advantage of the CorPath system is its mobility. According to Wenderow, a hospital with six cath labs could get away with having three systems — one system for every two rooms. This way, Wenderow explained, as one case wraps-up, the system can be wheeled into the adjacent room, the Bedside Unit manipulators replaced, and the system prepared for the next case in a matter of minutes. In contrast, the Stereotaxis system is permanently installed in the cath lab, which requires the cath lab to be retrofitted for installation and shut down for at least a month to make room for the system's two large magnets. Additionally, the system costs over $2 million--about 25 times the cost of a single CorPath unit. “A hospital with four labs loses one-fourth of its throughput for at least 30 days with the installation of a Stereotaxis system,” Wenderow pointed out.
Wenderow noted that the Stereotaxis system differs from CorPath in that the Stereotaxis system allows the magnetic wires to be “pulled” across a lesion instead of being “pushed” across, however, he indicated that a PCI started with a Stereotaxis system must be finished manually because the operator cannot deliver or deploy a stent.
Angioplasty And Beyond!
According to Wenderow, future iterations of the CorPath system might include applications for electrophysiology, neuron-vascular, and peripheral vascular procedures. “We believe that other areas of endovascular medicine and electrophysiology would also benefit from having a CorPath-like system at their disposal.”
“As the director of the Cath Lab and Interventional Cardiology, I see the potential for scalability and the system's application beyond angioplasty,” said Steven Bailey, MD, FACC (University of Texas Health Science Center in San Antonio, TX), who attended the ICI meeting.
Dr. Bailey stated that Corindus' indication for coronary angioplasty is only the tip of the iceberg; he sees the system being used for other applications such as placing pace-maker leads, where both precise positioning and discrete device movement are needed.


 November 24, 2025
November 24, 2025