March 5, 2023 — In patients with multi-vessel heart disease who have had a heart attack, immediate treatment with stents in all diseased arteries was found to be as safe and effective at one year of follow-up as staged treatment, according to findings from the first large, randomized trial to address this question that is being presented at the American College of Cardiology’s Annual Scientific Session Together With the World Congress of Cardiology. In staged treatment, the blocked artery that caused the heart attack is treated with a stent immediately and other partially blocked arteries are treated in a second procedure up to six weeks later.
About half of patients who have a heart attack have multi-vessel heart disease—this means that in addition to having one completely blocked coronary artery that caused their heart attack, they have additional narrowed coronary arteries that are at risk of becoming blocked or unstable, leading to another heart attack. Clinicians refer to the blocked artery that causes a heart attack as the “culprit lesion” and to the other at-risk arteries as “non-culprit lesions.”
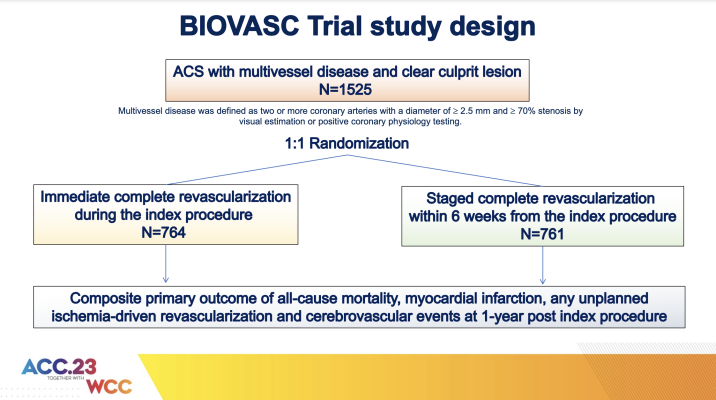
“The purpose of the international, randomized BIOVASC trial was to compare outcomes for immediate and staged complete revascularization for patients with multi-vessel heart disease who have suffered a heart attack. The goal was not to determine which approach was superior but rather to establish whether immediate complete vascularization was ‘not inferior’ to the staged approach, which needed to be answered first,” said Roberto Diletti, MD, PhD, an interventional cardiologist at Erasmus Medical Center in Rotterdam, Netherlands, and lead author of the study.
“We show that, at one year of follow-up, immediate complete revascularization is not inferior to staged complete revascularization for the study’s primary endpoint—that means that patients had similar rate of the composite of all-cause mortality, myocardial infarction, any unplanned ischemia-driven revascularization and cerebrovascular events,” Diletti said. “Moreover, immediate complete treatment offered reassurance that patients would not suffer a second heart attack while waiting for their second procedure.”
Stenting, also known as coronary angioplasty or percutaneous coronary intervention (PCI), is a minimally invasive procedure in which a flexible tube (catheter) is threaded through a coronary artery under local anesthesia. At the site of the blockage, a tiny balloon at the tip of the catheter is inflated to unblock the artery and a stent, a tiny mesh tube coated with medication, is implanted to prop the artery open, restoring blood flow to the heart.
The placement of stents in both “culprit” and “non-culprit” arteries is known as “complete revascularization.” Previous studies have shown that patients with multi-vessel heart disease have better outcomes when they undergo complete revascularization compared with stenting of the culprit artery alone. An unanswered question, however, has been whether outcomes are better when patients undergo a single procedure to place stents in both culprit and nonculprit arteries (immediate complete revascularization) or two procedures days or weeks apart (staged complete revascularization).
Clinicians have tended to favor the staged approach, Diletti said, because some observational studies have suggested that patients treated with immediate complete revascularization had worse outcomes. However, a risk of the staged approach is that the patient could have a second heart attack during the period before the second procedure. Expert guidelines currently state that the optimal timing for performing complete revascularization is unknown, he said.
In this study, a total of 1,525 patients (median age 65, 78% male) were enrolled in the trial in four European countries (Belgium, Italy, the Netherlands and Spain). Patients were randomly assigned to receive either immediate or staged complete revascularization. Among patients assigned to the staged treatment group, the second procedure could be performed later during the same hospital stay or at any time up to six weeks after the initial procedure. The study’s primary endpoint was a combination of death from any cause, another heart attack, any unplanned additional stenting procedures or cerebrovascular events at one year of follow-up. “Unplanned procedures” excluded staged stenting procedures in patients assigned to that arm of the study.
Among 1,506 patients at one year of follow-up, 7.6% of patients in the immediate complete revascularization group had a primary endpoint event compared with 9.4% of those who received a staged procedure. More than twice as many patients in the staged treatment group (4.5%) had a second heart attack than in the immediate treatment group (1.9%). Over 40% of the heart attacks in patients in the staged treatment group occurred during the interval before their second stenting procedure, Diletti said. The median interval between procedures for patients in the staged treatment group was 15 days.
Unplanned additional stenting procedures were more frequent among patients in the staged treatment group (6.7%) compared with the immediate treatment group (4.2%), a significant difference. The rate of stroke was similar in the two groups (1.5% in the immediate treatment group versus 1.6% in the staged treatment group). The median hospital stay was one day shorter for patients in the immediate complete revascularization group than for those whose procedure was staged.
The study findings were consistent across subgroups of patients, such as women versus men, younger versus older patients and patients with obesity versus those with weight in the normal range.
A limitation of the study is that both patients and their clinicians knew what treatment they were assigned to receive. In addition, a “real world” concern relates to clinicians’ willingness to perform immediate complete revascularization on patients hospitalized with an acute heart attack during “off” hours, Diletti said. Stenting of a patient’s non-culprit arteries could take anywhere from a few minutes to an hour and a half longer than treating the culprit artery alone, he said, depending on how many additional arteries need treatment and the complexity of the arterial blockages.
Diletti and his colleagues are currently analyzing data on patients’ quality of life following immediate or staged treatment. This analysis will not be covered as part of the ACC.23/WCC presentation and will be published separately. In addition, the research team will continue to follow the patients in the study for a total of five years.
The study was funded by a grant from Biotronik Inc. This study was simultaneously published online in The Lancet at the time of presentation.
For more information: www.acc.org


 July 31, 2024
July 31, 2024 









