Findings from the TRILUMINATE Pivotal trial in patients with a poorly functioning tricuspid valve in the heart, a minimally invasive procedure using a clip to repair the valve was safe and improved both the valve’s functioning and patients’ quality of life at one year compared with the best available medical therapy. The study also found no significant difference in survival or hospitalization after one year of follow-up, according to research presented on the first day of the American College of Cardiology’s Annual Scientific Session Together with the World Congress of Cardiology, ACC.23/WCC.
March 4, 2023 — Findings from the TRILUMINATE Pivotal Trial found no significant difference in survival or hospitalization after one year of follow-up, according to research presented on the first day of the American College of Cardiology’s Annual Scientific Session Together with the World Congress of Cardiology ACC.23/WCC. A presentation of findings during the first Late Breaking session reported that in patients with a poorly functioning tricuspid valve in the heart, a minimally invasive procedure using a clip to repair the valve was safe and improved both the valve’s functioning and patients’ quality of life at one year compared with the best available medical therapy, but did not show any significant difference in survival or heart failure hospitalization.
The ongoing international randomized clinical trial, known as TRILUMINATE Pivotal, is the first to evaluate the impact of improved tricuspid valve functioning on survival, heart failure hospitalizations and quality of life in patients with tricuspid valve regurgitation, according to the researchers. A summary of findings released by ACC, with portions shared here, also noted that analyses were performed by Abbott Laboratories.
“Patients with tricuspid regurgitation, when treated with transcatheter edge-to-edge repair (TEER) with the TriClip device, experienced significant improvements in quality of life,” said Paul Sorajja, MD, chair of the Valve Science Center at the Minneapolis Heart Institute Foundation (Minn, MN) and lead author of the study. Sorajja emphasized, “In a patient population with a high symptom burden, this is a meaningful benefit.”
TEER is a minimally invasive procedure in which a catheter (a long flexible tube) is used to place one or more tiny clips on the tricuspid valve leaflets to prevent blood from leaking back into the right atrium. The TRILUMINATE Pivotal trial was designed to determine whether patients with isolated tricuspid regurgitation would benefit from the procedure. The trial consisted of both a randomized cohort in which patients were randomly assigned to receive TEER or to continue with the best available medical therapy, and a single-arm cohort in which all patients received TEER. Patients deemed highly likely to achieve a reduction in tricuspid regurgitation to moderate or less were enrolled in the randomized trial; those deemed to have a low likelihood of achieving this level of reduction were enrolled in the single-arm trial, in which all patients were treated with TEER. The current study reports the results of the randomized trial.
A total of 350 patients (median age 78 years, 55% women) in five countries (U.S., Canada, Germany, Italy and Spain) were enrolled in the randomized trial. All patients had severe tricuspid regurgitation and heart failure symptoms despite receiving the best available medical therapy; 51% had tricuspid regurgitation rated as “torrential” (the highest level of severity on a five-level scale). Most patients also had either atrial fibrillation (an irregular, often very rapid heart rhythm) or high blood pressure, or both. In addition, all patients were at intermediate or higher risk for complications from tricuspid valve surgery. Patients who had severe left ventricular heart failure, untreated other valvular disease or severe pulmonary hypertension were not eligible to enroll.
After one year of follow-up, patients in the TEER group saw significant improvements in quality-of-life scores (average increase of 12.3 points) compared with control patients (average increase of one point). However, the primary endpoint itself wasn't met because there were no significant differences between the TEER and control groups in the number of deaths from any cause or the rate of hospitalization for heart failure. At 30 days, 87% of patients undergoing TEER had moderate or less tricuspid regurgitation, compared with 4.8% of those in the control group. Three patients (1.7%) had a major adverse event at 30 days (one death due to a cardiovascular cause and two cases of new kidney failure). Nine patients treated with TEER (5.2%) experienced a major bleeding event within one year. Five patients in the TEER group (2.9%) and five in the control group (2.9%) needed surgery to implant a permanent pacemaker or defibrillator within one year.
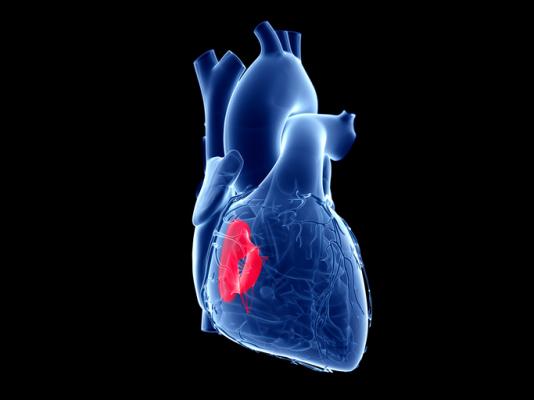
The authors noted that the tricuspid valve, one of four valves in the heart, controls blood flow from the heart’s upper right chamber, the right atrium, to the lower right chamber, the right ventricle. Tricuspid regurgitation occurs when the valve leaks, allowing blood to flow back into the right atrium. When this happens, the heart must work harder to pump blood effectively. Patients with severe tricuspid regurgitation frequently have symptoms such as severe fatigue and shortness of breath, an enlarged liver, kidney failure and fluid accumulation in the abdomen, legs, ankles or feet.
Tricuspid regurgitation may have many causes, such as dysfunction of the leaflets, or segments, of the tricuspid valve; atrial arrhythmias; failure of the left ventricle (the heart’s main pumping chamber); high blood pressure in the lungs (pulmonary hypertension); or it may be “isolated,” meaning that patients do not also have high blood pressure in the lungs or severe co-existing disease affecting the left side of the heart. Currently, the best available medical therapy for tricuspid regurgitation consists of diuretic medications that reduce fluid buildup in the body but often do not directly treat the mechanical leakage of blood through the tricuspid valve, Sorajja said. As a result, he said, patients with tricuspid regurgitation usually have poor quality of life.
The TRILUMINATE Pivotal trial will continue to follow the patients for five years. The study was funded by Abbott, maker of the TriClip device. Abbott also participated in site selection, trial management, data collection and analyses of the data. This study was simultaneously published online in the New England Journal of Medicine at the time of presentation.
Sorajja and other presenters of the ACC.23/WCC late-breaking clinical trial session were introduced by Valentin Fuster, MD, PhD, Editor-in-Chief of the Journal of the American College of Cardiology (JACC), President, Mount Sinai Heart, and Physician-in-Chief of The Mount Sinai Hospital (NY, NY). Fuster was introduced by ACC President Ed Fry, MD, Chair of the Ascension National Cardiovascular Service Line (Indianapolis, IN).
More information: acc.org


 February 04, 2026
February 04, 2026