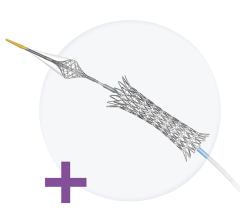
April 1, 2008 — Early results of the SPIRIT II study showed that the XIENCE V sstent was superior to the Taxus stent in six-month findings on angiography and trended better on one- year clinical outcomes. Now, a new analysis shows that after two years, the investigational everolimus- coated XIENCE V stent may continue to hold a clinical edge over its paclitaxel-coated competitor.
The two-year findings of the SPIRIT II study are being reported today in a Late-Breaking Clinical Trials session at the SCAI Annual Scientific Sessions in Partnership with ACC i2 Summit (SCAI-ACCi2) in Chicago. SCAI-ACCi2 is a scientific meeting for practicing cardiovascular interventionalists sponsored
by the Society for Cardiovascular Angiography and Interventions (SCAI) in partnership with the American College of Cardiology (ACC).
Patrick W. Serruys, M.D., Thoraxcenter, Erasmus Medical Center, Rotterdam, The Netherlands, led the SPIRIT II study. He and his colleagues recruited 300 patients from 28 medical centers in Europe, New Zealand and India who needed stenting of up to two new coronary lesions. Patients were randomly assigned to treatment with the XIENCE V everolimus-eluting stent or the Taxus paclitaxel-eluting stent.
The study primarily set out to document any differences in the amount of arterial tissue that grew into the stents at six months (in-stent late loss). As previously reported, the results were significantly better for the XIENCE V stent when compared to the Taxus stent. At one-year follow-up, the combined rates
of major adverse cardiac events (MACE), consisting of cardiac death, heart attack and repeat procedure to treat the target lesion, trended better in the XIENCE V group.
New data from a late-stage evaluation report demonstrates that the XIENCE V stent continues to show a trend toward improved clinical outcomes compared to the Taxus stent at two years, however, the trial was not statistically powered to show differences in clinical endpoints. The overall MACE rate at two
years was 40 percent lower in patients treated with the XIENCE V stent (6.6 percent vs. 11.0 percent in the Taxus group). Repeat procedures to treat the target lesion were performed in 3.8 percent and 6.8 percent of patients, respectively, a 44 percent reduction favoring the XIENCE V stent. Similarly, the
rates of heart attack were 2.8 percent and 5.5 percent, respectively, a 49 percent reduction, and the rates of cardiac death were 0.5 percent and 1.4 percent, respectively, a 64 percent reduction. There was no difference in the rates of blood clotting inside the stent, or stent thrombosis, at two years.
In the 117 patients who had follow-up angiography at two years, there was no significant difference in the rates of re-narrowing of at least 50 percent (binary restenosis) within the stents (2.1 percent with the XIENCE V stent vs. 2.9 percent with the Taxus stent). In-stent late loss was virtually identical (0.33 mm
vs. 0.34 mm, on average, respectively).
For more information: www.scai-acci2.org


 November 24, 2025
November 24, 2025