April 20, 2011 – Patients who have aneurysms, stroke, heart rhythm disorders, cholesterol build up in arteries and numerous other cardiovascular and neurovascular diseases will benefit from new technology now in place at Methodist University Hospital. The technology produces 3-D images that are faster and more accurate, and that aid advanced surgery and treatments. Methodist University Hospital is the first mid-South hospital and among a few hospitals in the United States, to offer this technology housed in its new Neurovascular and Cardiovascular Center.
“The Artis zeego and the Artis biplane technology are the new gold standard for academic cardiovascular and neurovascular care. It gives us the most advanced care available for our patients,” said Kevin M. Spiegel, FACHE, CEO, Methodist University Hospital. “It is better and safer and it will give us the ability to save more lives.”
The system’s robotic C-arm allows physicians to move the imaging system instead of the patient, allowing virtually unrestricted positioning. It reduces strain on the patient while helping improve treatment by gathering images from a variety of positions that were previously difficult to obtain.
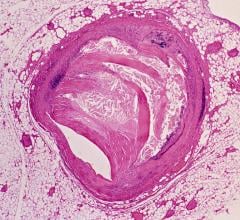
The CT-type images are needed to guide physicians through arteries during tedious procedures, such as implanting stents to repair an abdominal aortic aneurysm, repairing a brain aneurysm or correcting heart rhythm problems.
“It is wonderful to have this latest technology to offer my patients,” said James Porterfield, M.D., director of electrophysiology laboratory at Methodist University Hospital. “In my 30 years of experience, this is the most exciting era for medical advancements.”
Lower radiation exposure to patients and their care team is another benefit, because it allows physicians to image larger portions of the body at one time.
“The opening of this cutting edge imaging-interventional system and hybrid room is timed perfectly as we begin a new fellowship training program in interventional cardiology at UT and Methodist,” said Guy L. Reed, M.D., Lemuel Diggs Professor of Medicine and chairman of the department of medicine, University of Tennessee Health Science Center.
The Artis zeego also positions Methodist University Hospital to perform minimally invasive percutaneous valve repair, once a device for that procedure is approved by the FDA.
Percutaneous valve procedures are an alternative to traditional open-heart surgery and are being performed via clinical trials at a few places around the country, most notably Columbia University Medical Center. A new prosthetic valve may be on the market later this year.
Valve Clinics to Open
Methodist is opening two valve clinics to identify patients with aortic valve stenosis (narrowing) who may be candidates for the procedure. The clinics will be located at Sutherland Cardiology in Memphis and on the campus of Methodist University Hospital in the Memphis medical center. University of Tennessee Health Science Center’s UT Medical Group will be involved in the clinic in the medical center. Patients who are candidates will travel with their local valve clinic physicians for surgery at a site where the surgery is offered.
“Aortic stenosis is so undertreated,” said Jeffrey Gibson, M.D. with The CardioVascular Center. “Through our evaluation process in the valve clinic, we will be able to give some patients with this condition a new treatment option.”
“Minimally-invasive percutaneous valve repair is a landmark innovation in cardiac care,” said Santosh K.G. Koshy, M.D., interventional cardiologist with UT Medical Group and an associate professor of cardiology at the University of Tennessee Health Science Center. “At the valve clinic, this remarkable new procedure will be a welcome option for many patients.”
“This exciting technology gives us the ability to reverse the damage caused by stroke in selected cases,” said Adam Arthur, M.D., a neurosurgeon with Semmes-Murphey Neurologic and Spine Institute and assistant professor of neurosurgery at the University of Tennessee Health Science Center. “We will be able to help a lot of patients suffering from both bleeding within the brain and those with blockages in important arteries.”
The Artis zee biplane imaging system features an advanced software technology that creates detailed images of soft tissue, such as brain tissue, which helps detect intracranial hemorrhages, visualize brain tissue and enable physicians to make quick and accurate therapeutic decisions. This saves critical time for stroke patients by providing physicians highly detailed anatomical images directly in the interventional suite, so they can immediately begin interventional treatment.
This technology will be used for minimally invasive neurovascular procedures such as clot removal, aneurysm repair, the treatment of arteriovenous malformations, carotid artery blockages, brain and neck tumors, and intracranial hemorrhages.
“The window of opportunity for intervention for stroke patients can be expanded from three hours to eight hours for certain patients who have a stroke caused from a clot,” said Arthur. “These five additional hours will enable us to reduce disability and the risk of death from stroke.”
This new technology features advanced X-ray detectors that provide the sharpest and clearest high-resolution images in three-dimensions from any direction without the distortion common with conventional x-ray techniques. The detectors also help physicians visualize interventional devices, such as guide wires and catheters, in precise detail and from almost any angle.
Low dose radiation and the ergonomic design of the system eliminate time-consuming and uncomfortable repositioning of the patient in the exam room, making procedures faster and less stressful for the patient. This technology also reduces the length of a procedure by at least 50 percent, thus reducing risk to the patient from the amount of radiological dye used.
For more information: www.methodisthealth.org


 October 24, 2025
October 24, 2025