Although not a new technology, optical coherence tomography (OCT) is the dark horse of imaging that could give traditional angiography and intravascular ultrasound a run for its money as interventional cardiologists look for new ways to improve patient outcomes when performing percutaneous coronary intervention (PCI).
Angiograms were first adopted by cardiologists after Dr. Mason Sones Jr. accidentally injected contrast dye into his patient’s small arteries back in 1958. Since then it has become the standard imaging tool used by interventional cardiologists for treating patients with coronary artery diseases. Cardiac catheterization labs are designed around this practice of imaging, and interventional cardiologists have become the experts at interpreting the shadows produced by the X-ray images they see. Although the practice of interventional cardiology has advanced over the last 60 years, the fundamentals of angiography have remained essentially the same.
OCT might be able to improve patient outcomes by allowing much more detailed, high resolution views inside the coronary vessels than what is allowed by angiography.
Application of Optical Coherence Tomography in the Cath Lab
Here in the United States, Abbott Vascular acquired the OCT technology through St. Jude Medical in 2017, which had purchased LightLab, the original manufacturer of the coronary imaging tool.
Using laser technology, OCT captures high-resolution images of the inside of the patient’s arteries, displaying the type of disease and coronary artery dimensions in great detail to determine how the patient should be treated.
Physicians can use OCT to assess and understand the degree of disease and take necessary steps to treat it. With highly accurate measurements, OCT can be used to guide target lesion assessment, vessel prep and device selection, with subsequent placement and deployment (e.g., expansion and apposition) as well as determine how well the stent was placed in the vessel. Immediate evaluation of apposition can lead to precision stenting with unsurpassable accuracy.
LightLab Clinical Initiative Aims to Understand The Barriers to OCT Adoption
The LightLab Clinical Initiative is a multiphase program that examines the role and impact of OCT imaging when used to guide PCI. The aim of the initiative is to understand the many barriers to routine adoption of OCT in PCI procedures. Its findings can drive future software development to optimize the utility of the information and workflow in PCI.
The initiative is taking place at 12 medical centers across the United States, including our clinic at the Kansas Heart Hospital and Ascension Via Christi St Francis Hospital. This initiative seeks to gather the data necessary to assess if a pre-scripted workflow (MLD MAX) can uncover improvements in decision making accuracy, efficiency and reductions in contrast use and radiation.
In order to better understand what it takes to adopt OCT in the cath lab, field clinical engineers are present at these medical centers to facilitate the use of this workflow and collect procedural data, as doctors are performing percutaneous coronary interventions on their patients. This will quantify real-world parameters in decision making and efficiency during procedures when doctors are following the LightLab OCT workflow.
3 Key Takeaways for OCT at EuroPCR
At this point in time, the first phase of LightLab has concluded. The findings were presented at the EuroPCR 2020 eCourse, and revealed that physicians altered their treatment strategy in 88% of coronary artery blockages based on new information provided by OCT over and above angiography. This statistic alone has enormous implications for our day-to-day practice.
There were three key takeaways for us following this first phase of the initiative:
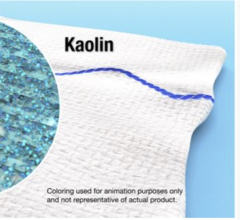
1. While one could argue that the high percentage of changes in physician decision-making through OCT-guided PCI was provoked by the large amount of information provided by OCT, many of the changes involved key procedural information and decisions. For example, the correct assessment of the presence of calcification drives target lesion prep and, how it results in utilizing more efficient and less time-consuming treatment
2. As we know, stent expansion is a big driver of PCI outcomes; by following the pre-scripted steps to assess lesion diameter and length, we were able to more accurately estimate and select the right stent size.
3. Although the LightLab Clinical Initiative is still in the early stages, OCT-guided PCI has already begun to demonstrate its clinical and practical utility as it provided us with the right data at the right time, creating the conditions to select and place stents with greater precision.
We look forward to seeing what the capabilities of OCT uncover as the subsequent phases of the LightLab Initiative continue. The next phase in the initiative focuses on what effect the LightLab OCT workflow will have on efficiency, cost and safety gains during PCI procedures—something to which all of us as practitioners can relate.
Editor’s note: The authors of this article are Aziz Maksoud M.D., FACC, FSCAI, and Bassem Chehab, M.D., FACC, FSCAI.
Maksoud is a graduate of the American University of Beirut Medical School and the University of Kansas internal medicine residency program as well as cardiovascular fellowship program, and he concluded his training at the University of Connecticut interventional fellowship program at the Hartford Hospital. Since then, Maksoud has been in practice with the Cardiovascular Consultants of Kansas in Wichita, Kans. In 2016, he and Chehab started the Cardiovascular Research Institute of Kansas which, Maksoud also chairs.
Chehab finished his fellowship in Interventional cardiology and cardiovascular medicine at the University of Kansas Medical Center in Kansas City. He completed his residency in internal medicine at the University of Kansas. Chehab is board certified in internal medicine and in cardiovascular medicine and is a member in multiple professional medical societies. With a long and extensive research tract, Chehab worked on multiple pivotal clinical trials and research projects. He is the director of the structural cardiology program and Center of Excellence for Heart Valve Therapy at Ascension Via Christi Hospitals in Wichita, Kan.


 March 17, 2025
March 17, 2025