Bare metal stents (BMS) were introduced in 1994 as an improvement over balloon angioplasty alone, which had a high restenosis rate of between 30-40 percent. The cobalt-chromium or stainless steel stents helped reduce restenosis, bringing rates down to about 15-20 percent, but BMS also increased the risk of early in-stent thrombosis shortly following the procedure. The thrombosis is controlled using anti-platelet therapy with ticlopidine, clopidogrel or prasugrel. However, BMS are not immune from restenosis, primarily by neointimal hyperplasia caused from the ripping of the vessel during balloon expansion and exposure of the vessel’s smooth muscle cells.
To overcome the neointima scar tissue, drug-eluting stents (DES) were introduced in the United States with Cypher (Cordis) in 2003 and Taxus (Boston Scientific) in 2004. They were followed by Endeavor (Medtronic), Xience (Abbott) and Promus (Boston Scientific) in 2008. Drug-eluting stents (DES) use the same anti-proliferation drugs used to fight cancerous tumors, including sirolimus (Cypher), paclitaxel (Taxus), everolimus (Xience, Promus), and zotarolimus (Endeavor).
Most DES elute their drug in the first three months, which is the period when scar tissue typically forms in bare metal stents. Endeavor elutes in about two weeks, Cypher in about 100 days, and Xience and Promus well after 100 days. Experts will debate if it is better to elute most of the drug early during the initial vessel healing process, or if it is better to elute smaller doses over a longer period of time.
While DES significantly reduce restenosis compared to BMS rates, studies found DES have increased rates of late-stent thrombosis, believed to be caused by the drug delivery polymer irritating the vessel. The rate of thrombosis is below 1 percent, but this finding prompted the American College of Cardiology to post guidelines suggesting 12 months of anti-platelet therapy after DES implantation.
Anti-platelet drugs have their own side effects and hamper other medical or dental procedures because it increases bleeding. To eliminate the need for extended anti-platelet use and the dangers of late-stent thrombosis, manufacturers are developing bioabsorbable polymers. The first stents in this class that are likely to gain FDA approval include Boston Scientific’s JACTAX and the Cordis Nevo. Nevo also uses tiny holes in the struts as drug polymer reservoirs to cut the amount of polymer on the stent and its contact with the vessel wall. JACTAX uses dots of polymer along the struts to limit vessel/polymer contact.
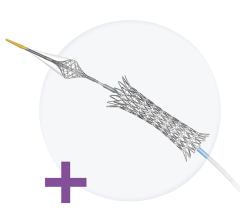
Abbott plans to take the concept a step further with its totally bioabsorbable BVS stent, now in its third year of European clinical trials. While Abbott is the furthest along with this technology, the BVS would not likely gain FDA approval until the middle of the next decade.
Manufacturers are experimenting with specially-treated stent surfaces, allowing the drug to be directly applied without a polymer. Neointimal hyperplasia can also be prevented if exposed smooth muscle cells are quickly covered over by a layer of endothelial cells. Some stents in development use coatings to promote re-endothelialization.
Noncoronary Stents
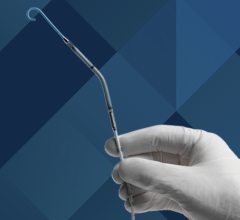
With the overwhelming success of coronary stenting came interest in using the same technology to treat other vessels, especially the carotid and renal arteries, and peripheral artery disease (PAD) affecting the femoral, popliteal and iliac arteries.
PAD affects nearly 10 million Americans, many of whom are not treated, or are treated with surgery. Frost & Sullivan estimates this is the largest area of growth for stents in the coming years. The healthcare research firm said revenues for peripheral stenting in 2006 were about $161 million, and it estimates it will reach about $376 million by 2013. In comparison, the U.S. market for coronary stents alone is currently about $500 million annually. Some estimates put the worldwide PAD stent market at about $1 billion by 2012.
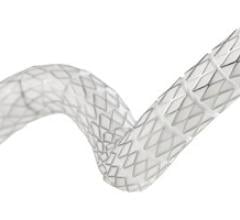
PAD stents need more flexibility than coronary stents because lesions can be much longer and are located between muscle and bone in the legs, where they are put under stress and torque. This can displace, fracture and crush conventional stents, especially in vessels below the knee. For this reason many peripheral stents are self-expanding, made of flexible nitinol (nickel-titanium alloy, developed by the Naval Ordinance Lab), which can bend and reshape to its original form.
Specialty stents are also being developed for strokes and aneurisms.
Stent Characteristics
Experts say stents need to be judged on the basic criteria of deliverability, safety and efficacy. Other features for comparison include visibility under X-ray, scaffolding design for more effective drug elution and easier deliverability, securement to balloons so stent is not lost on the way to the blockage, and the conformity of the stent struts to the vessel walls (apposition) when expanded. Other factors include radial strength to prevent stent strut recoil and the loss of lumen size, biocompatibility of the metal and polymers used, and the amount of foreshortening upon deployment (stents are longer on a balloon, but shorten when they are expanded).
The design of struts, cross members and strut thickness may influence fluid dynamics inside a vessel, which is believed to be a factor in plaque formation. Some manufactures say thinner struts may aid in re-endothelialization. Both thickness and strut design can influence stent deliverability, including its flexibility and fiction on the vessel walls. Strut spacing can impact the amount of vessel wall coverage and the drug delivery effectiveness.


 November 24, 2025
November 24, 2025