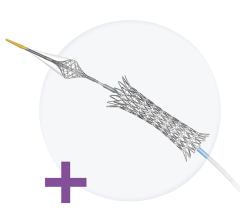
The Cook Zilver PTX self-expanding stent may become the first drug-eluting stent available in the United States if it is cleared by the FDA later this year.
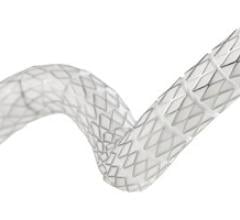
The goal of treating peripheral artery disease (PAD) in the superficial femoral artery (SFA) is limb salvage and improving quality of life. However, these arteries are among the toughest in the body to maintain patency, and repeat interventions are very common. Percutaneous transluminal angioplasty (PTA) is primarily used, but has high restenosis rates, and the environment is not suitable for balloon-expanded stents.
However, a drug-eluting, self-expanding stent that does not use a drug-carrier polymer is before the U.S. Food and Drug Administration (FDA) final pre-market approval (PMA) review and a decision is expected later this year. Its chances of approval appear very bright, considering its positive clinical trial data to date.
Two-year data from the Zilver PTX Trial was presented in January at the 23rd annual International Symposium on Endovascular Therapy (ISET). The multicenter, prospective, randomized trial includes a total of 479 patients treated at 55 institutions. About half received the Cook Medical Zilver PTX paclitaxel-coated stent and the rest received angioplasty alone to open blocked SFAs. Patients who received angioplasty that did not succeed in initially opening the artery were then randomized to a provisional group to receive either paclitaxel-coated or bare-metal stents (BMS).
Two-year data included 278 patients, with approximately 50 percent getting the Zilver PTX stent, 25 percent getting angioplasty alone, 12.5 percent getting angioplasty plus provisional bare metal stent and 12.5 percent getting angioplasty plus provisional Zilver PTX stent. After two years, 74.8 percent of arteries remained open in patients who received the drug-coated stents. There was no imaging of the angioplasty-only group after the first year, at which point only 32.8 percent had arteries that remained open. After two years, event-free survival was 86.6 percent for Zilver PTX patients. Events that did occur primarily involved the need to undergo another procedure to open the original blockage, worsening symptoms of PAD and one amputation. No patient deaths were related to the study device or procedure.
In the provisional stenting group at two years, 81.2 percent of arteries treated with drug-coated stents remained opened vs. 62.7 percent of those treated with bare-metal stents.
“We are very excited about the Zilver PTX,” said Rob Lyles, vice president and global leader of Cook Medical’s peripheral intervention business unit. “It represents a huge step forward in terms of peripheral disease – it’s a step beyond bare metal stents.”
At one year, vessel patency with balloon angioplasty alone in leg vessels is 30-35 percent and with BMS it is about 65-70 percent. At one-year, the Zilver offers patency of 80-90 percent. “One of the obvious problems is that the outcomes in these vessels are not that great,” Lyles said. “This is a huge step forward.”
At two years, the Zilver PTX stent showed a 50 percent reduction in restenosis over angioplasty. This is significant because previous peripheral DES trials showed positive outcomes at 12-18 months, but then restenosis rates began to rise.
Lyles said the increase in restenosis (23 percent at two years) in the SIROCCO trial for the Cordis sirolimus-eluting, self-expanding Smart Stent was due to a high stent fracture rate (19 percent in SIROCCO I, 10.7 percent stent fracture rate in SIROCCO II). The SIROCCO II study showed DES delay, but failed to prevent restenosis in the SFA. Smart Stent and a BMS version of the Smart Stent were compared and were about equal in outcomes, but the DES version had a slightly higher restenosis rate of about 23 percent at two years.
The STRIDES trial for Abbott’s Dynalink-E everolimus-eluting, self-expanding stent had a lower fracture rate of 1.8 percent, but, possibly due to the drug used, it did not offer lasting benefits after 12 months, Lyles said.
The Zilver PTX has a fracture rate of only 0.9 percent.
Another advantage of the Zilver over previous DES is it does not use polymer to retain and control drug elution. Instead, the paclitaxel is applied with a special lipophilic coating. It is immediately absorbed when the stent contacts the vessel wall when the stent is deployed from a sheath. Unlike olimus drugs, paclitaxel has the ability to rapidly absorb into tissue, and its anti-proliferative effects are long-lasting.
Trial data also shows the Zilver PTX performs just as well in diabetics as it does in non-diabetics, which may be due to the use of paclitaxel.
If approved, it will be the first DES cleared in the U.S. that does use a polymer.


 November 24, 2025
November 24, 2025