In a move that will likely have a significant impact on how many patients are treated for carotid artery disease, the U.S. Food and Drug Administration (FDA) in May cleared the use of a stent to treat standard-risk surgical patients. Prior to this approval, carotid stenting was only indicated for used in high-risk surgical patients who were often denied the standard-of-care of carotid endarterectomy surgery.
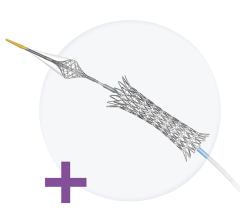
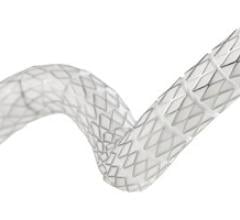
The decision to expand the indication for the Abbott RX Acculink carotid stent system is expected to have a major impact, offering patients the option of minimally invasive stenting rather than open surgery, which often leaves scars on the patient’s neck.
The RX Acculink was cleared in 2004 for patients at high risk of adverse events from surgery. The stent is used in combination with the RX Accunet Embolic Protection System and is the first stenting system cleared for use in standard-risk patients for the treatment of carotid artery disease.
“Expanded access to RX Acculink means patients and their healthcare providers have another option for treating clogged neck arteries,” said Christy Foreman, MBE, director of the Office of Device Evaluation in the FDA’s Center for Devices and Radiological Health.
The FDA expanded the stent’s indications based on the results of the CREST (Carotid Revascularization Endarterectomy vs. Stenting Trial) study. The 10-year CREST study included 2,502 patients at 119 clinical sites in the United States and Canada. Patients were treated and followed for at least one year. The National Institutes of Health helped to fund the study, which found that patients treated with RX Acculink had a similar combined rate of death, stroke and heart attack (myocardial infarction) as those who underwent surgery.
“The CREST data demonstrated that carotid artery stenting is a safe, effective and minimally invasive treatment for standard-risk patients with carotid artery disease,” said L. N. Hopkins, M.D., professor and chairman, department of neurosurgery, and professor of radiology, State University of New York at Buffalo. “With this broader indication, the RX Acculink carotid stent system will become an important option for physicians as they determine the most appropriate treatment approach for their patients.”
An outside expert advisory panel convened by the FDA on Jan. 26, 2011, found the RX Acculink to be generally safe and effective for use in this new group of patients. But the panel emphasized the need for additional long-term follow-up information and the importance of the stent’s use in conjunction with an embolic protection device to capture plaque and other debris that break away during the procedure, potentially causing a stroke.
As a condition of the approval, the manufacturer, Abbott Vascular, is required to conduct a post-approval study, which will follow new patients treated with RX Acculink for at least three years to confirm the results identified in the pre-market study. The post-approval study will also evaluate how patients age 80 years and older respond to treatment, whether treatment success is affected by the physician’s experience with the product and whether patients who show symptoms of having a clogged carotid artery experience a different outcome than those who don’t show any symptoms prior to treatment. The study is planned to assess clinical outcomes at 30 days and annually for three years. This study is consistent with recommendations made by the expert advisory panel.
Offering Patients a Choice
“The CREST trial results showed us it is really a matter of choice, it’s not really showing any superiority between stenting and endarterectomy,” said Christopher White, M.D., FSCAI, FACC, FAHA, FESC, system chairman for cardiovascular diseases, Ochsner Heart and Vascular Institute, Ochsner Medical Institutions, New Orleans, and president of the Society of Cardiovascular Angiography and Interventions (SCAI). “These are everyday patients who are now offered the alternative of carotid stenting. It’s what’s best for the patients and up until now, we could not always do what was best.”
While he is a big fan of stenting, he points out CREST showed stenting is not the best option for all patients, due to tortuous anatomy or because of of a heavily calcified aortic arch. He said a computed tomography (CT) or magnetic resonance imaging (MRI) screening is always needed to evaluate these factors to determine the best option for each patient.
“There are still some reasons why stenting will not replace endarterectomy,” White said. “We really should match our patients to the best therapy that suits them.”
“FDA approval of the RX Acculink carotid stent system for patients at standard risk of surgery has the potential to significantly impact the treatment of patients with carotid artery disease,” said Charles A. Simonton, M.D., FACC, FSCAI, divisional vice president, medical affairs, and chief medical officer, Abbott Vascular. “More than 60 percent of U.S. patients with carotid artery disease are at standard surgical risk, many of whom require a procedure to open the narrowed arteries that lead to the brain. This expanded indication for Abbott’s RX Acculink provides these patients with an additional treatment option.”
Impact on Physicians
Over the past decade, vascular surgeons have embraced interventional procedures, so any increase in carotid stenting volume will probably not reduce their patient volume. He said the best approach is for surgeons and interventional cardiologists to work together in evaluating patients to determine the best course of treatment.
If stenting does increase, White warns that only experienced operators at higher volume centers should perform carotid stenting. He said CREST screened all its operators to ensure they were all highly experienced in carotid stenting. “It’s not just the procedure, outcomes also depend on the experience of the operator,” White said, explaining low-volume centers should not being performing these complex procedures.
Reimbursement is Next Hurdle
Abbott said it plans to use the CREST trial data to ask the Centers for Medicare and Medicaid Services (CMS) to reimburse carotid stenting. Even with the FDA’s endorsement, CMS has refused to reimburse carotid stenting in high-risk surgical patients.
“This has been a struggle, and the next step will be to get CMS to accept it for Medicare funding,” White said. “Without reimbursement, it really is just a hollow approval.”
Since most carotid artery disease patients are over the age of 60, Medicare funding will be a key factor in determining if carotid stenting sees a rapid expansion, White explained.


 November 24, 2025
November 24, 2025