When vessels are stretched and ripped via angioplasty balloon expansion, the exposed soft muscle tissue can lead to the proliferation of scar tissue (neointimal hyperplasia) that can reocclude the vessel. Drug-eluting stents (DES) were introduced in 2003 to overcome this issue with anti-proliferative drugs, the same as used to prevent cellular growth in cancerous tumors. However, the drug-eluting polymer coatings have caused concern about late-stent thrombosis. The required long-term use of dual anti-platelet therapy also carries risks of increased bleeding and hampers other medical and dental procedures.
Experts seem to agree one of the keys to reducing restenosis and stent thrombosis is to cover the stent and the exposed smooth muscle tissue with a new layer of endothelial cells. These cells naturally coat the vessel lumen. Promoting this early neointimal cellular growth is hampered by anti-proliferative drugs.
Stent manufacturers say the goal of DES is to prevent the neointimal hyperplasia that usually occurs in the first months following PCI, but then hope for the benefits of the biocompatibility of a bare metal stent in allowing the vessel to heal over the long term.
A few companies are developing alternatives to DES with stent coatings to speed the growth of neointimal cells. While the development of the next step in DES technology with bioabsorbable polymers and totally bioabsorbable stents is exciting, the development of stents with endothelial progeneration properties is something that also merits close watch.
Stents Promoting Re-Endothelialization
CeloNova BioSciences developed the CE-marked Catania stent, coated with a polyzene-F microfilm that has anti-inflammatory properties to help accelerate vessel healing. The company said the surface treatment is an inorganic polymer that confers superior biocompatibility and lubricity to the substrates it coats. The stent allows anti-platelet therapy to end after 30 days, the company said.
The stent is being evaluated in the REVEAL study, where patients were randomized to receive a Catania stent, and either a CYPHER, TAXUS, or a bare metal stent. At seven days, optical coherence tomography showed the Catania had better endothelial cell strut coverage than the other stents, and at 30 days Catania had fewer uncovered struts than the DES, but not the BMS.
The one-year data for the first-in-man presented at the TCT 2008 showed no stent thrombosis, death, myocardial infarction, stroke, or coronary artery bypass graft.
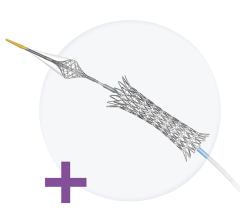
OrbusNeich is developing the Genous Bioengineered R Stent. It is coated with immobilized antibodies (CD34+) that capture circulating endothelial progenitor cells (EPC) to promote rapid endothelialization. The stent is being used in several studies overseas and some findings were presented at TCT and AHA in 2008 suggesting good clinical outcomes with low rates of TVR and no late-stent thrombosis.
One-year outcomes of a 1,640 patient international study showed low rates for restenosis, target lesion revascularization (5.4 percent), and in-stent thrombosis (1 percent).
The Federico II University of Naples’s Division of Cardiology, Department of Clinical Medicine and Cardiovascular Sciences, presented data on its 257 high-risk patients who underwent PCI with either the Genous, TAXUS or CYPHER stent. After PCI, patients who received a Genous stent were prescribed dual anti-platelet therapy for one month, and patients who received DES were prescribed the same therapy for 12 months. At 13 months the cumulative MACE rate for the Genous group was 17.2 percent versus 26.4 percent for the combined TAXUS and CYPHER group – a 35 percent reduction. For the MACE components, the rate of myocardial infarction was 4.5 percent for Genous, versus 6.8 percent for DES. The revascularization rate was 7.5 percent for Genous and 13.5 percent for TAXUS and CYPHER. The cardiac death rate was 4.5 percent for Genous versus 7.4 percent for the DES stents. In addition, the rate for stent thrombosis was zero percent for Genous, versus 5.8 percent for DES.
In November 2008 Global Therapeutics initiated a clinical trial using the GTX bare metal stent coated with an anti-sense RNA therapeutic agent aimed at silencing one of the genes (c-myc) responsible for causing restenosis. Once implanted, the stent sheds its drug coating, leaving behind a bare metal stent after 24 hours. The drug stays in the tissue for more than two weeks, the company said.
Hexacath developed the BAS (Bio Active Stent) TITAN2 coated with titanium-nitride-oxide and NO-particles as an alternative to DES. The TITAN2 BAS has demonstrated its exceptional behavior in clinical results through various studies enrolling more than 1,700 patients. The company says its Titanox coating provides the highest biocompatibility and hemocompatibility ever achieved with any stent, and does not contain potentially inflammatory substances such as nickel, cobalt or polymer. The TITAN registry showed no MACE or thrombosis at 30 days. At 180 days MACE was reported at 3 percent and there was zero thrombosis.


 November 24, 2025
November 24, 2025