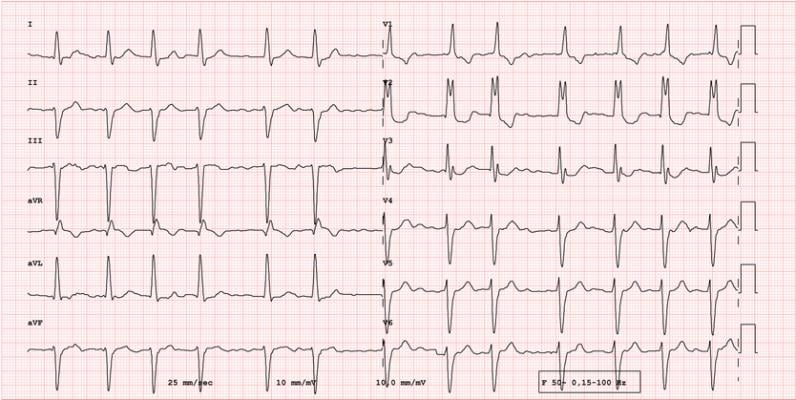
During its Annual Conference, HRS 2024, the Heart Rhythm Society (HRS) announced findings from three new studies demonstrating the safety and efficacy of pulsed field ablation (PFA), a nonthermal ablation treatment for patients with atrial fibrillation (AF). See full findings from the FARADISE, admIRE Study, and Advent Trial here. Image courtesy: Getty Images
May 18, 2024 — The Heart Rhythm Society (HRS) has announced the findings of three new studies demonstrating the safety and efficacy of pulsed field ablation (PFA), a nonthermal ablation treatment for patients with atrial fibrillation (AFib). PFA shortens operating times and may reduce the chance of damage to surrounding tissues with high safety margins. Researchers presented these findings as late-breaking clinical science during Heart Rhythm 2024 (HRS 2024), being held May 16-19 in Boston, MA.
Atrial fibrillation is the most common type of arrhythmia, and by 2050, up to 16 million Americans are projected to have AF1. Contemporary guidelines recommend antiarrhythmic drugs as the initial therapy for the maintenance of sinus rhythm, but these medications are associated with serious adverse events2. Catheter ablation (thermal ablation or PFA) is an effective nonpharmacological alternative that is often, but not always, the second-line treatment if long-term medications or electrical cardioversion are not preferred or are not effective. PFA is different from thermal ablation — which has stood as the standard ablation method for AF for decades—in that it disables cardiac cells using electricity instead of heat or extreme cold. Recent technological advancements, such as catheter design and energy delivery, can pave the way for the wider adoption of PFA in clinical practice to improve patient outcomes.3
The findings of the following studies contribute to the growing body of evidence supporting PFA as an effective treatment option for patients with AF.
Real-world data collection in subjects treated with the FARAPULSE Pulsed Field Ablation system (FARADISE)
FARADISE is a global, prospective, post-market registry that studied real-world outcomes in more than 1,000 patients to demonstrate the safety and effectiveness of the FARAPULSE PFA System, which uses an over-the-wire catheter with variable distal shapes (basket and flower). The findings were presented during an HRS Late-breaking science session held May 17, “Late Breaking Clinical Trials and Science - Ablation: Real world data collection in subjects treated with the FARAPULSE Pulsed Field Ablation system (FARADISE).” A summary of findings, as presented in a written update from HRS, follow.
At 3 and 6 months after ablation in patients with paroxysmal and non-paroxysmal AF, researchers did not observe any reported deaths or certain serious complications, including coronary spasm, persistent phrenic nerve palsy, atrio-esophageal fistula, or pulmonary vein stenosis. Compared to traditional thermal catheter ablation, the FARAPULSE PFA System requires a significantly shorter duration of energy application. Pulmonary vein isolation (PVI) procedure, left atrial dwell, and fluoroscopy times were 51, 32, and 12 minutes, respectively.
For patients with additional ablation beyond PVI, average procedure, left atrial dwell, and fluoroscopy times were 68, 42, and 16 minutes, respectively. “Acute outcomes presented from more than 1,000 patients in the global FARADISE registry reinforce the safety, efficacy and efficiency profile of the FARAPULSE PFA System for the treatment of atrial fibrillation, with no reports of coronary spasm, pulmonary vein stenosis, persistent phrenic nerve palsy or esophageal fistula,” said Prof. Lucas Boersma, electrophysiologist, St. Antonius Hospital, Netherlands, professor of electrophysiology, Amsterdam UMC, and lead investigator of the FARADISE registry. “We look forward to gathering long-term evidence from this registry for this particular PFA therapy, which continues to generate promising outcomes in real-world use.”
Long-term Safety and Effectiveness After Paroxysmal Atrial Fibrillation Pulsed Field Ablation from the U.S. Multicenter admIRE Study
The admIRE study, a prospective, multicenter, single-arm clinical trial, sought to demonstrate the safety and efficacy of the VARIPULSE PFA Platform when used for isolation of pulmonary veins in treatment of patients in the United States with symptomatic drug refractory paroxysmal AF. Findings were shared during a May 17 late-breaking science session, “Late Breaking Clinical Trials and Science - Ablation: Long-term Safety and Effectiveness After Paroxysmal Atrial Fibrillation Pulsed Field Ablation from the U.S. Multicenter admIRE Study.” Summary findings follow, as presented in a written statement from HRS after the presentation.
All patients in the study achieved acute success. Participants also saw a significant improvement in quality of life and reduced healthcare utilizations in terms of cardiovascular hospitalizations, cardioversion, and antiarrhythmic drug use. These results demonstrate the VARIPULSE PFA Platform can offer safe, consistent, and effective therapy, which may expand accessibility for patients seeking AF ablation and allow better early rhythm control.
“The admIRE study demonstrated good safety and effectiveness results. The primary effectiveness success was 74.6%, and among the subset of participants receiving 73-96 PFA applications for PVI, 85% achieved success. Primary safety events occurred in 2.9%, demonstrating promising evidence of the capabilities of the VARIPLUSE Platform,” said Vivek Reddy, M.D., director of electrophysiology, Mount Sinai Fuster Heart Hospital, New York. He added, “Differentiated by its unique CARTO 3 System integration, this was the first PFA investigational device exemption study to support a substantial number of fluoro-free procedures; 25% of procedures were performed with zero fluoroscopy.”
Impact of Pulsed Field vs Thermal Ablation on One-Year Atrial Arrhythmia Burden – Sub-analysis of the ADVENT Trial
Recent evidence indicates that post-ablation atrial arrhythmia (AA) burden – the total duration of atrial fibrillation patients experience – is a better predictor of clinical outcomes than the standard 30-second definition. Results presented in a late-breaking session,
“Late Breaking Clinical Trials and Science - Ablation: Impact of Pulsed Field vs Thermal Ablation on One-Year Atrial Arrhythmia Burden – Sub-analysis of the ADVENT Trial,” held on May 18 and shared by HRS in a written statement are shared here.
Data from the ADVENT randomized controlled trial, which compared the safety and effectiveness of the FARAPULSE PFA System to standard thermal ablation, sought to determine if residual AA burden affected quality of life (QoL), clinical outcomes, and if these outcomes differed between ablation modalities. After weekly post-ablation transtelephonic ECG monitoring (TTM) and 72-hour Holter monitor readings at 6 and 12 months, researchers found that patients treated with the FARAPULSE PFA System demonstrated a statistically superior reduction in arrhythmia burden (0.1% AA burden.
“Treatment with the FARAPULSE PFA System achieved a clinically meaningful, low residual AA burden compared to traditional thermal ablation, with positive impacts on quality of life and clinical outcomes for patients,” said Dr. Reddy. “This data provides novel, helpful evidence for predicting the patient clinical experience and comparing the effectiveness of this therapy to standard thermal ablation for pulmonary vein isolation,” added Reddy. Researchers presented these trials at respective late-breaking clinical trial sessions on Friday, May 17, and Saturday, May 18.
The Heart Rhythm Society's annual Heart Rhythm meeting convenes 8,500+ of the world’s finest clinicians, scientists, researchers, and innovators in the field of cardiac pacing and electrophysiology. More than 1,500 international experts in the field will serve as faculty and presenters for the 200+ educational sessions, forums, symposia, and ceremonies, while 120+ exhibitors will showcase innovative products and services.
The Heart Rhythm Society is the international leader in science, education, and advocacy for cardiac arrhythmia professionals and patients and is the primary information resource on heart rhythm disorders. Its mission is to improve the care of patients by promoting research, education, and optimal health care policies and standards. Incorporated in 1979 and based in Washington, D.C., it has a membership of more than 8,000 heart rhythm professionals from 94 countries.
For more information, www.HeartRhythm.com
Follow DAIC for more HRS 2024 news coverage here.
Reference:
1Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. Journal of American Medical Association, 2001; 285:2370- 2370. doi:10.1001/jama.285.18.2370
2 Andrade JG. Ablation as First-line Therapy for Atrial Fibrillation. Eur Cardiol. 2023;18:e46. doi: 10.15420/ecr.2023.04.
3 Iyengar SK, Iyengar S, Srivathsan K. The promise of pulsed field ablation and the challenges ahead. Front Cardiovasc Med., 2023;10:1235317. doi:10.3389/fcvm.2023.1235317.

 June 08, 2023
June 08, 2023 

