Results of the IMPLEMENT-HF Trial show that a virtual care team-guided strategy for guideline-directed medical therapy (GDMT) optimization was found to be safe and improve therapy among patients hospitalized with heart failure with reduced ejection fraction (HFrEF). Findings were presented during a Featured Clinical Research session on the final day of the American College of Cardiology Annual Scientific Session Together with the World Congress of Cardiology, ACC23 WCC, being held March 4-6 in New Orleans, LA.
March 7, 2023 — A virtual care team-guided strategy for guideline-directed medical therapy (GDMT) optimization was found to be safe and improve therapy among patients hospitalized with heart failure with reduced ejection fraction (HFrEF), according to a multicenter implementation trial presented at ACC.23/WCC and simultaneously published in the Journal of the American College of Cardiology, JACC.
Findings were presented on the final day of the American College of Cardiology's Annual Scientific Session Together with the World Congress of Cardiology, ACC.23/WCC, by Ankeet S. Bhatt, MD, MBA, MSc. Bhatt, who presented significant findings from “Safety and Efficacy of Virtual Care Team Guided Therapeutic Optimization During Hospitalization in Patients with HFrEF: the IMPLEMENT-HF Study.” Bhatt is currently a Critical Care Cardiologist and Research Scientist/Investigator with Kaiser Permanente Division of Research (Oakland, CA), previously at Massachusetts General/Brigham & Women’s Hospital (Boston, MA), which funded the study.
In the study, Bhatt et al assessed the safety and effectiveness of a virtual care team-guided strategy on GDMT use in hospitalized patients with HFrEF.
“The virtual care team strategy was safe with no increase in adverse events, and the beneficial effects did not come at the expense of increasing hospital length of stay. All in all, virtual care teams represent an effective, scalable and safe approach to have FREF therapeutic optimization. I'd love to thank our large team without which this would not have been possible. And I'm very happy to report that these findings are now simultaneously published in JACC,” said Bhatt in concluding his presentation of findings during the March 6 Featured Clinical Research Session III on March 6 at ACC23/WCC in New Orleans.
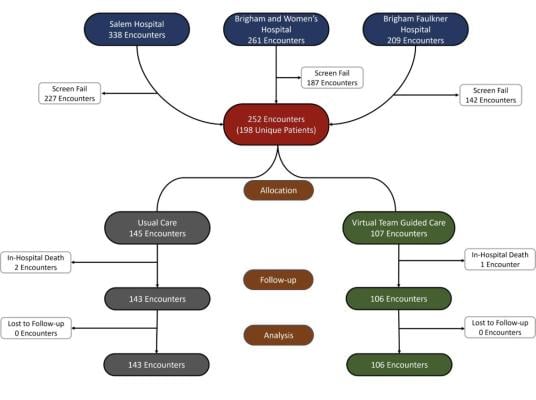
The researchers allocated patients with a left ventricular EF ≤40% to a virtual care team-guided strategy (107 encounters among 83 patients) or usual care (145 encounters among 115 patients). The patients were from three centers in an integrated health care delivery system. Their mean age was 69 years, 34% were women, 14% Black and 17% Hispanic.
Clinicians in the virtual care team group received up to once daily recommendations for optimizing GDMT from a physician-pharmacist team. The primary goal was to improve early treatment of four major drugs classes (beta-blockers; ACE inhibitors/ ARB/ ARNI; mineralocorticoid receptor antagonists; SGLT2i). Effectiveness was measured by the in-hospital change in the optimization score (+2 initiations, +1 dose uptitrations, –1 downtitrations, –2 discontinuations summed across classes), and in-hospital safety outcomes were analyzed by an independent clinical events committee.
Results showed that GDMT optimization scores improved with the virtual care team strategy vs. usual care (adjusted difference +1.2; 95% CI, 0.7-1.8; p<0.001). In these groups respectively, there was a higher rate of new initiation of GDMT (44% vs. 23%; p=0.001) and intensifications of ≥one GDMT 50% vs. 28%; p=0.001). This translated to a number-needed-to-intervene of five encounters to optimize GDMT during hospitalization.
In terms of safety outcomes, there was no significant excess in adjudicated serious adverse events (21% vs. 28%) in the intervention and control groups, respectively, had one or more safety events (p=0.30), with similar rates of acute kidney injury, bradycardia, hypotension and hyperkalemia.
The study authors emphasized the benefits of the tested platform being fully virtual. They write, “This strategy represents a potential highly effective, scalable intervention that can lead to accelerated implementation of guideline concordant HFrEF care.”
In summarizing the findings, Bhatt reviewed the results: Among 252 encounters, mean age was 69±14 years, 85(34%) were women, 35(14%) were Black, and 43(17%) were Hispanic. The virtual care team strategy significantly improved GDMT scores vs. usual care (adjusted difference +1.2;95% CI:0.7-1.8;P<0.001). New initiations (44% vs.23%;P=0.001) and intensifications of ≥1 GDMT (50% vs.28%;P=0.001) were higher in the virtual care team group, translating to a number-needed-to-intervene of 5 encounters. Overall, 23(21%) in virtual care team group and 40(28%) in usual care experienced 1 or more safety events(P=0.30). AKI, bradycardia, hypotension, and hyperkalemia were similar between groups.
Among patients hospitalized with HFrEF, a virtual care team-guided strategy for GDMT optimization was safe and improved GDMT across multiple hospitals in an integrated health system. Virtual teams represent a centralized, scalable approach to optimize GDMT.
For more information: www.acc.org


 February 04, 2026
February 04, 2026