November 9, 2018 — The American College of Cardiology (ACC), the American Heart Association (AHA) and the Heart Rhythm Society (HRS) released a guideline for the evaluation and treatment of patients with bradycardia, or a slow heartbeat, and cardiac conduction disorders.
In the guideline, bradycardia is defined as a heart rate of less than 50 beats per minute, compared to a normal heart rate of 50-100 beats per minute. A slow heartbeat can limit the amount of blood and oxygen that is pumped to all the organs of the body. Bradycardia is generally classified into three categories — sinus node dysfunction, atrioventricular (AV) block and conduction disorders. In sinus node dysfunction, the sinoatrial node, the main pacemaker of the heart, cannot maintain an adequate heart rate. In AV block, there is partial or complete interruption of electrical impulse transmission from the atria to the ventricles. Cardiac conduction disorders occur when electrical impulses in the heart that cause it to beat are delayed. Common conduction disorders include right and left bundle branch block. Bradycardia and conduction abnormalities are more often seen in elderly patients.
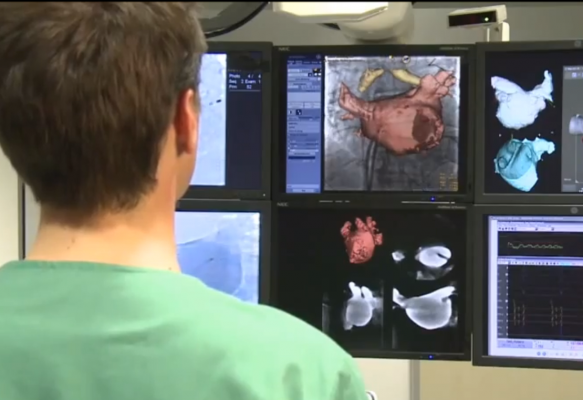
In the guideline, the writing committee members outline the clinical presentation and approach to clinical evaluation of patients who may have bradycardia or conduction diseases. They reviewed study data and developed recommendations from the evidence. These recommendations include the selection and timing of diagnostic testing tools — including monitoring devices and electrophysiological testing — as well as available treatment options such as lifestyle interventions, pharmacotherapy, and external and implanted devices, particularly pacing devices. The authors also address special considerations for different populations based on age, comorbidities or other relevant factors.
Conduction abnormalities are common after transcatheter aortic valve replacement (TAVR). The guideline includes recommendations on post-procedure surveillance and pacemaker implantation. The guideline also addresses ways to approach the discontinuation of pacemaker therapy and end of life considerations.
The writing committee members stress the importance of shared decision-making between the patient and clinicians, as well as patient-centered care.
“Treatment decisions are based not only on the best available evidence but also on the patient’s goals of care and preferences,” said Fred M. Kusumoto, M.D., cardiologist at Mayo Clinic Florida in Jacksonville and chair of the writing committee. “Patients should be referred to trusted material to aid in their understanding and awareness of the consequences and risks of any proposed action.”
Yet, according to the authors, there are still knowledge gaps in understanding how to manage bradycardia, especially the evolving role of and developing technology for pacing.
“Identifying patient populations who will benefit the most from emerging pacing technologies, such as His bundle pacing and transcatheter leadless pacing systems, will require further investigation as these modalities are incorporated into clinical practice,” Kusumoto said. “Regardless of technology, for the foreseeable future, pacing therapy requires implantation of a medical device, and future studies are warranted to focus on the long-term implications associated with lifelong therapy.”
The 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay are published online in the Journal of the American College of Cardiology, Circulation, journal of the American Heart Association and HeartRhythm.
For more information: www.ahajournals.org/journal/circ; www.onlinejacc.org; www.heartrhythmjournal.com


 November 12, 2025
November 12, 2025 









