July 17, 2015 - NeoStem Inc. presented updated efficacy and safety results from the one-year follow-up for its Phase 2 PreSERVE study and additional analyses of certain functional tests at the American College of Cardiology's 64th annual scientific session and expo in March. The one-year follow-up results are defined as all data accumulated until the last patient enrolled completed 12-month follow-up. Thus, the results actually represent data from patients with a median follow-up of 18 months.
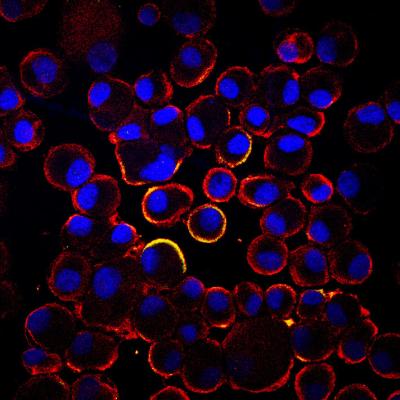
NeoStem is developing CD34 cell-based therapies to address damage to tissue caused by ischemia. Ischemia occurs when the supply of oxygenated blood in the body is restricted. The company's Ischemic Repair Program seeks to reverse the damage caused by this restriction through the development and formation of new blood vessels. The program's lead product candidate in this area is NBS10, a chemotactic hematopoietic stem cell product comprised of autologous bone marrow-derived CD34/CXCR4 cells selected to treat damaged heart muscle following acute myocardial infarction (AMI).
One-year follow-up safety data collected thus far supports the trial's six-month results presented at the American Heart Association's scientific sessions in November 2014. The ACC presentation contained updated safety and exploratory efficacy data and additional analyses conducted on left ventricular ejection fraction (LVEF) data.
Clinical Endpoint Committee adjudication of major adverse cardiac events (MACE) was performed on the six-month data reported previously and was not performed for new events (occurring between 6 and 12 months). The next prescribed adjudication of MACE is currently planned at the end of patient follow-up. At 12-month follow-up, no meaningful safety or tolerance differences were observed between treatment and control groups. In this updated analysis, no additional deaths were reported in the treatment or control groups beyond those previously reported in the six-month analysis. In addition, in post hoc subset analyses based on the number of cells patients received, serious adverse event (SAE) frequency continues to show numerical improvement at all cell doses when compared to control.
No additional single-photon emission computed tomography (SPECT) data were collected at one year follow-up. As an exploratory measure of efficacy, PreSERVE looked at reduction of infarct size at six months. Patients receiving 20 million cells or more experienced a decrease in infarct size of 41 percent versus 24 percent for patients in the control group.
Based on the one-year follow-up results, the company and its scientific advisors believe that the study results suggest:
- Intracoronary administration of autologous CD34+ cells appears safe and well-tolerated;
- A signal for a mortality benefit; and
- A signal for reduction in the frequency of serious adverse events (SAEs) in higher dose groups.
"While small in number, we are encouraged by the fewer mortality events observed for treated patients versus control patients as of the date of this 12-month follow-up. In addition, we are very encouraged by the persistence of reduced serious adverse event rates and evidence for improved infarct healing and left ventricular function," said Arshed A. Quyyumi, M.D., professor of medicine at Emory University and lead principal investigator of the PreSERVE AMI study, who made the presentation at ACC.15. "In addition, the failure of SPECT imaging to document changes at the 6 month interim analysis, despite signs of clinical benefit in multiple parameters, suggests that this technique is not applicable in this setting."
For more information: www.neostem.com


 February 03, 2026
February 03, 2026 









