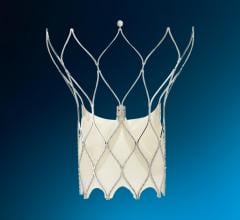
The Watchman device is a transcatheter left atrial appendage occluder. It is meant to be an alternative to blood thinners in preventing stroke in patients with atrial fibrillation.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and is a major risk factor for developing emboli leading to stroke. A new approach to preventing embolisms and stroke is the use of percutaneous occlusion of the left atrial appendage (LAA).
Atrial Fibrillation
AF is the most common sustained cardiac arrhythmia affecting about 2.2 million people in America and 4.5 million in Europe. The prevalence of AF increases with age from 3-5 percent in people older than 65 years to more than 10 percent in people over age 80. The incidence of AF is noted to follow a similar pattern, with an exponential increase to 20-30 per 1,000 patient-years in people older than 85 years of age. It is estimated as many as 15.9 million adults will be affected with AF by the year 2050.
AF is frequently associated with structural heart disease, particularly in the developing countries where rheumatic valvular disease is prevalent. In the Western countries, medical conditions such as hypertension, diabetes, congestive heart failure and atherosclerotic heart disease are key risk factors for the development of AF. It increases the risk of stroke mortality and morbidity. The risk of thromboembolic stroke is increased three-to-five fold in people with nonvalvular AF. Stroke risk, based on the Framingham Heart Study, increased 17-fold in AF patients with rheumatic heart disease when compared with age-matched controls.
The prevalence of AF and stroke increases with age independently. The annual risk of stroke attributed to AF in the Framingham Study was 1.5 percent in patients ages 50 to 59, and about 23 percent in patients over 80. In addition to stroke, AF is associated with an increased risk of heart failure and all-cause mortality.
Limits of Anticoagulation Therapy
Currently oral anticoagulation therapy with warfarin is the mainstay of therapy in patients with atrial fibrillation, but has been found to have significant limitations. Warfarin is a medication with a very narrow therapeutic window — too much increases the likelihood of major bleeding dramatically. Too little, and the therapeutic effect is lost, placing the patient at increased risk for thromboembolic complications. It is therefore no surprise that a search for alternative treatments, both pharmaceutical as well as interventional, has been an active area of research for many years. One area of intense interest has been in the area of left atrial appendage (LAA) exclusion.
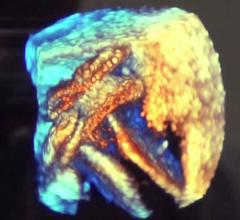
Excluding the LAA From Circulation
Ever since it was first discovered the LAA was the main source of emboli in more than 90 percent of patients with nonvalvular AF, the idea of excluding it from the systemic circulation has been studied. The first reported case of surgical excision of the left atrial appendage for atrial fibrillation was performed in a canine model in 1947 by Herman K. Hellerstein, M.D., which was followed by the first two cases in man in 1949 by John L. Madden, M.D.. Since that time, surgical exclusion of the LAA during coronary artery bypass graft (CABG) surgery has been widely accepted, with retrospective studies of single center experiences suggesting that the practice is both safe and effective.
However, in the ongoing Left Atrial Appendage Occlusion Study (LAAOS), where patients with atrial fibrillation and undergoing CABG are randomized 2:1 to LAA exclusion or not, results of the pilot study have been less than stellar. Complete exclusion of the LAA was achieved in only 45 percent of patients undergoing excision with suturing, and in only 72 percent of patients in whom a stapler was used.
Surgical exclusion of the LAA as a stand-alone procedure has not gained wide acceptance for obvious reasons. Techniques utilizing minimally invasive techniques such as thoracoscopy have been described, but the technique is still in its infancy.
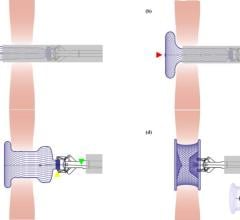
Transcatheter LAA Occlusion
One promising approach that has recently been studied is percutaneous occlusion of the LAA via a trans-septal puncture from the femoral vein. The first trial examining this technique was the PLAATO Trial (2005) using a polytetrafluoroethylene (PTFE)-covered nitinol scaffold (made by ev3) designed to sit within the LAA. The PLAATO Trial was a phase I clinical trial that demonstrated a 97 percent success rate (108/111) for complete occlusion of the LAA documented on transesophageal echocardiogram (TEE), with a 61 percent relative risk reduction of the expected stroke rate based on historical controls. The procedure was associated with a significant learning curve and complications like tamponade and hemothorax, while rare, did occur.
More recently, the PROTECT-AF Trial (2007), utilizing the Watchman device from Atritech, demonstrated an 81 percent immediate success rate for LAA occlusion, which increased to 92 percent by six months. Overall stroke risk was noninferior to patients randomized to oral anticoagulation therapy with warfarin. As in the PLAATO Trial, patients undergoing implantation of the Watchman device had a significant (4.8 percent) risk of pericardial effusion and tamponade.
FDA Review, Market Clearance
So how close are we to a mechanical solution to nonvalvular atrial fibrillation? While the initial phase I trial of the PLAATO device demonstrated promising results, there are no plans to proceed with a phase II or III trial due to lack of funding. The PLAATO program was discontinued in 2005. In 2007, ev3 said it sold its intellectual property to Atritech to support its Watchman device.
The PROTECT – AF trial was met with great enthusiasm by the medical community when it was first presented at the 2009 American College of Cardiology (ACC) meeting. But achieving regulatory approval from the U.S. Food and Drug Administration (FDA) has proved to be more challenging.
The FDA’s Circulatory Systems Device Panel made a 7-5 recommendation of approval for the device to the FDA in April 2009. However, almost a year later in March 2010, the FDA has ruled that further clinical trials confirming the safety and efficacy of the device will be needed before final approval is granted.
New Device Set for Trial
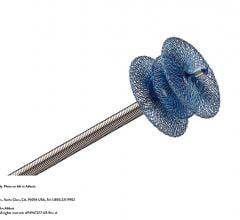
A third device from AGA, the Amplatzer Cardiac Plug, began its phase I clinical trial, after receiving a conditional investigational device exemption (IDE) approval from the FDA in March. The first patients are enrolled in the feasibility phase of the prospective, multicenter, randomized U.S. clinical trial, designed to evaluate this device.
Unfortunately, it seems that we are still several years away from getting these devices approved. But, if the clinical trials continue to demonstrate positive results, we will soon have a definitive treatment for the prevention of stroke in nonvalvular atrial fibrillation, which will help make oral anticoagulants a thing of the past.



 June 20, 2024
June 20, 2024