Anatomic eligibility for EVEREST II was sufficient leaflet tissue for mechanical coaptation and non-rheumatic/endocarditic valve morphology.
Preliminary results of a multicenter study show that the use of tiny clips to repair the mitral valve may someday eliminate the need for open-heart surgery for most sufferers of mitral regurgitation (MR).
Presented in April at the SCAI Annual Scientific Sessions in partnership with the ACC i2 Summit, data gathered over two years in the ongoing Edge-to-Edge REpair STudy (EVEREST) showed that of 23 patients with moderate-to-severe or severe functional mitral regurgitation (grade 3 to 4 ), 83 percent had noticeable MR reductions with 74 percent showing reductions below or at 2 after being treated with the MitraClip from Menlo Park, CA-based Evalve Inc.
In addition, 92 percent showed a stabilization or improvement of clinical symptoms at one year.
Furthermore, all patients spent an average of only three days in the hospital before being allowed to return home for self-care.
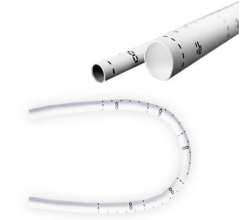
Unlike surgery, which requires that the heart be stopped in order to repair the mitral valve, the new percutaneous technique uses a V-shaped mitral clip that is put into place by using a catheter while the heart is still beating.
Seeking Solutions
With over 250,000 cases diagnosed each year, MR has become the most common type of heart valve dysfunction, characterized by improperly closing valve leaflets. The resulting leakage between the left atrium and left ventricle subsequently leads to chronic volume overload.
The pathology of MR was first described by Professor Alain Carpentier in 1983, and he is credited with developing a highly regarded surgical solution.
Depending on which leaflet is problematic, surgeons may resection the abnormal portion of the valve or perform a chordal transfer. New chords may also need to be created. In every case, though, an annuloplasty also is performed to cinch the rim of the valve. “Surgery is the gold standard,” said Howard Herrmann, M.D., director, interventional cardiology, cardiac cath labs, Hospital of the University of Pennsylvania, and an investigator in the EVEREST trials.
Advances in surgery have led to an even newer technique developed by Ottavio Alfieri, M.D., in which the free edge of the anterior leaflet is attached to the posterior leaflet in the area of mitral regurgitation. “[Dr.] Alfieri added a new tool to the toolbox,” Dr. Herrmann noted, adding that by stitching together the anterior and posterior leaflets, you create a dual orifice valve.
Patrick Whitlow, M.D., director of interventional cardiology at the Cleveland Clinic Foundation, and another EVEREST investigator, points out that the new mitral clip “mimics the Alfieri stitch.” He also said, “The clip is now the only alternative to surgery.”
Testing the Clip
The successful completion of Phase I clinical trials involving 27 patients led the way to recruiting patients for Phase II.
While Phase I tested the safety and efficacy of the procedure, Phase II is based on a 2:1 randomization to test the clip’s effectiveness against conventional mitral valve repair. It is being conducted at 30 medical centers across the U.S.
According to Ted Feldman, M.D., director of the cardiac cath lab at Evanston Northwestern Healthcare and co-principal investigator for EVEREST II, the patient selection criteria for
Phase II are stringent:
• 18 years old or older
• Moderate to severe (3 ) or severe (4 ) MR
• Symptomatic
• Asymptomatic with LVEF 40 mm
• MR originates from A2-P2 mal-coaptation
• Candidate for mitral valve surgery including CPB
• Transseptal deemed feasible
Key exclusions include:
• EF 55 mm
• Renal insufficiency
• Endocarditis, rheumatic heart disease
Dr. Feldman also noted, “A high risk registry has finished enrollment, but not follow up.”
Although Phase I trials were a success, some adverse events were reported. Both Drs. Herrmann and Whitlow acknowledge there were three instances where the clip detached from one of the leaflets. But in no case did they totally detach. “They did not embolize,” Dr. Herrmann said. “And they were successfully operated on.” No emergency surgeries were needed, he added.
He also states these incidences have led to a better understanding of the procedure to ensure that the clip is well-anchored to both leaflets. “Major complications have been amazingly low for a new technology,” he said. “It’s a safe and controlled procedure.”
Since the beginning of the EVEREST trials Dr. Herrmann says he’s installed one or more clips in 15 patients. “We’re reproducing the results seen in the trials nationally,” he said.
Dr. Whitlow has used the clips in about 20 patients, he said, adding, “The results have been very good.”
One patient who was scheduled for the percutaneous procedure had a heart that was too deformed, and another patient had such a severe leak that he opted to have elective surgery, Dr. Whitlow said.
Future Holds Promise
Because this procedure is performed by interventional cardiologists in the cath lab, there has been some discussion as to whether this will ultimately pit surgeons against cardiologists. But Dr. Whitlow says it could actually lead to more cooperation. “We have surgeons involved in the protocol,” he said. “And they’re learning to do minimally invasive techniques as well.”
Added Dr. Herrmann: “The proper approach is collaboration with the hope that a percutaneous procedure could minimize the potential adverse effects of surgery.”
Dr. Whitlow also says that if the leaflet repair consistently works well and lasts a long time, it could prove to be a viable alternative to surgery. But if the ventricle enlarges and the MR get worse, for example, “then we may consider using the clip and doing an annuloplasty,” he said.
The importance of mitral valve repair in lieu of replacement has spawned new interest among researchers and medical device companies. “There are more than a dozen companies investigating percutaneous MR solutions with five or six in clinical trials,” said Dr. Herrmann.
One casualty, however, has been a new device that was being developed by Irvine, CA-based Edwards Lifesciences LLC.
With Phase I clinical trials begun in Europe, the MOBIUS transcatheter repair program uses a steerable catheter through which a suture is inserted. Once either the anterior or posterior leaflet is stitched, the catheter is then rotated 180 degrees so that the edge of the opposite leaflet can likewise be stitched.
In July 2007, the company announced it was suspending all clinical trials on this new device.
Sarah Huoh, senior manager of global communications for Edwards Lifesciences, explained the end of testing, “After completing our clinical feasibility study, we determined that it would continue to take considerable additional resources and time to affect durable and long-lasting repair results with the MOBIUS device. Therefore, we’ve decided to redirect these resources into our other advanced technology development programs.”



 January 15, 2026
January 15, 2026