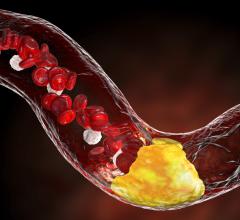
December 8, 2015 — Researchers from the University of Toronto have found that a specific cell type plays a key role in maintaining healthy arteries after inflammation. It’s a discovery that could provide treatment options for cardiovascular disease — one of the leading causes of death in Canada.
The researchers found that a specific type of tissue macrophage, a group of white blood cells that defend against infection, are created and operate separately from other macrophages that come from the bone marrow. Unlike bone marrow macrophages, these cells live in the outer layer of the arterial wall, can self-replicate and help to heal the vessel after inflammation.
“We’ve discovered that a group of macrophages are created when the embryo is developing, before the bone marrow is functioning,” said Clinton Robbins, a professor in the Faculty of Medicine’s Departments of Laboratory Medicine and Pathobiology and Immunology. “These macrophages can self-replicate and likely regulate the normal function of our arteries. This is a fundamental biological discovery that could play an important role in many cardiovascular diseases.”
The journal Nature Immunology published the results of the study.
Robbins and his team found that during infection these self-replicating macrophages leave the arterial wall, while macrophages from the bone marrow come in and engulf the bacteria. The team thinks that once inflammation resolves, the self-renewing macrophages return to heal the damaged tissue.
Using a special tagging system, they accurately traced where the macrophages were coming from.
“Previously, we couldn’t identify one macrophage from another because we were limited by technology,” said Robbins, who is also the Peter Munk Chair of Aortic Disease Research in the Toronto General Research Institute at University Health Network. “Now we can see exactly where they’re coming from and where they’re going. Our job now is to get a better understanding of what these different macrophage populations are doing.”
Next, the researchers will study how these resident macrophages interact with their tissue environment and exactly what role they might play in cardiovascular disease. By understanding the relationship between the different cell types, they hope to target inflammation caused by infection or atherosclerosis more effectively.
“We know that while bone marrow macrophages remove bacteria, they can also cause atherosclerosis by entering the arterial wall and multiplying,” said Rickvinder Besla, graduate student and co-lead author. “In the old model, you might try to shut the bone marrow response down, but this leaves the patient immunosuppressed. Our new model suggests we could possibly reduce inflammation by boosting the activity of these self-replicating macrophages.”
Robbins acknowledges that there’s still a lot to learn about the complexity of these macrophages and how they interact with their environment and other cells.
“Arteries are more than tubes that shuttle blood around. They create a complex and dynamic network that reacts to inflammation and disease in different ways. We’re excited to figure out another piece of this puzzle and how we might target cardiovascular disease in the future,” he said.
For more information: www.medicine.utoronto.ca


 November 12, 2025
November 12, 2025