June 13, 2019 — Silk Road Medical Inc. announced the presentation of real-world data for the treatment of patients with carotid artery disease at risk for stroke at the Society for Vascular Surgery 2019 Vascular Annual Meeting (VAM), June 12-15 in National Harbor, Md. In a headline presentation, Mahmoud Malas, M.D., of the University of California, San Diego School of Medicine shared updated results for the ongoing TransCarotid Artery Revascularization (TCAR) Surveillance Project.
“The results of the TCAR Surveillance Project are overwhelmingly positive on a large dataset of patients, showing, for the first time, significantly lower odds of composite in-hospital stroke, death and myocardial infarction compared to CEA [carotid endarterectomy]. TCAR had statistically equivalent in-hospital stroke and death rates as CEA, with significantly lower odds of myocardial infarction and cranial nerve injury. Additionally, there was a significant reduction in mortality at 30 days and 1 year, likely attributable to the reduction in myocardial infarction,” Malas said. “Patients clearly benefit from TCAR’s less-invasive approach and with these data and future studies with similar results, I believe TCAR may become the standard of care.”
The presentation, “Outcomes of Transcarotid Revascularization with Dynamic Flow Reversal Versus Carotid Endarterectomy in the Transcarotid Revascularization Surveillance Project,” evaluated patients between 2015 and 2018, with 5,716 patients receiving TCAR compared to 44,442 patients receiving carotid endarterectomy (CEA). Propensity score matching was used to analyze 5,160 patients in each group. There were no statistical differences noted between TCAR and CEA for in-hospital stroke (odds ratio (OR) 0.80, p=0.19) or in-hospital stroke and death (OR: 0.77, p=0.09).
Other key findings for TCAR compared to CEA include:
-
Fifty-nine (59) percent lower odds of in-hospital myocardial infarction (OR: 0.41, p<.001);
-
Eighty-seven (87) percent lower odds of in-hospital cranial nerve injury (OR: 0.13, p<0.001);
-
Thirty-five (35) percent lower odds of in-hospital stroke, death and myocardial infarction (OR: 0.65, p<.01);
-
Twenty-six (26) percent lower odds of hospital stay longer than 1 day (OR: 0.74, p<0.001); and
-
Twenty-five (25) percent lower odds of non-home discharge (OR: 0.75, p<0.001).
In a separate risk adjusted analysis looking at 30-day and one-year followup, the results were as follows:
-
Thirty-four (34) percent lower odds of 30-day death (OR: 0.66, p=0.03);
-
Forty-six (46) percent lower odds of 30-day stroke and death (OR: 0.54, p=0.02);
-
Fifty-three (53) percent lower odds of 30-day stroke, death and MI (OR: 0.47, p<0.01);
-
Twenty-three (23) percent lower odds of 1-year mortality (OR: 0.77, p=0.02).
The TCAR Surveillance Project, a key initiative of the Society for Vascular Surgery’s Vascular Quality Initiative (VQI), is an open-ended registry intended to compare real-world patient outcomes between TCAR and CEA.
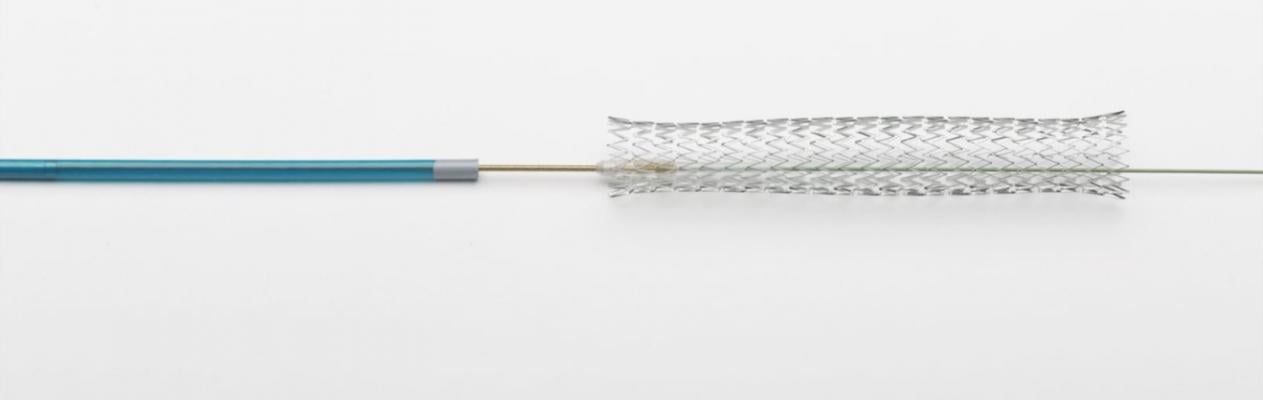
TCAR (TransCarotid Artery Revascularization) is a clinically proven procedure combining surgical principles of neuroprotection with minimally invasive endovascular techniques to treat blockages in the carotid artery at risk of causing a stroke. The Enroute Transcarotid Stent is intended to be used in conjunction with the Enroute Transcarotid Neuroprotection System (NPS) during the TCAR procedure. The Enroute Transcarotid NPS is a first-in-class device used to directly access the common carotid artery and initiate high rate temporary blood flow reversal to protect the brain from stroke while delivering and implanting the Enroute Transcarotid Stent.
For more information: www.silkroadmed.com


 January 05, 2026
January 05, 2026 









