March 7, 2012 — Four leading heart organizations representing cardiologists and cardiothoracic surgeons released initial recommendations for creating and maintaining transcatheter aortic valve replacement (TAVR) programs. The recommendations are aimed at ensuring optimal care for patients with aortic stenosis, a form of valvular heart disease, as use of the new TAVR procedure grows.
Since the U.S. Food and Drug Administration’s (FDA) approval of TAVR in November 2011, interest in the procedure has quickly grown among cardiologists and cardiothoracic surgeons as well as patients, prompting efforts by professional medical societies to identify institutional and physician credentialing criteria for performing the procedure. The published recommendations represent a joint collaboration of cardiovascular specialty societies, including the American College of Cardiology Foundation (ACCF), the Society for Cardiovascular Angiography and Interventions (SCAI), the American Association for Thoracic Surgery (AATS) and the Society for Thoracic Surgeons (STS).
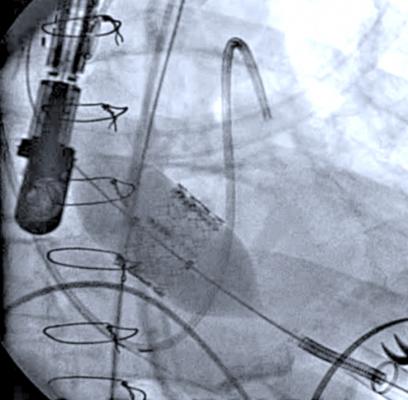
TAVR is a minimally invasive procedure found by the FDA to be reasonably safe and effective in the treatment of patients with severe aortic stenosis who cannot undergo surgery and have the absence of comorbidities, as described in the FDA label. Prior to the availability of TAVR, patients had few, if any, treatment options for aortic stenosis, which can lead to heart failure and death. During TAVR, physicians use a catheter to thread the replacement valve from a blood vessel in the groin to the heart's diseased aortic valve, which is then replaced with the new valve.
"As new technologies begin to be incorporated into cardiovascular practice, it is the responsibility of the medical societies to work together to develop standards for optimal patient care," said Carl Tommaso, M.D., chair of the document writing committee and medical director of the cardiac catheterization lab, Skokie Hospital, NorthShore HealthSystem, Chicago. "TAVR is a complex procedure that has potential to serve many patients, and it is up to us to deliver the highest standard of care available."
Due to the complexity of the procedure and the rapid rate at which the technology is evolving, defining operator and institutional requirements is a vital step in ensuring optimal program implementation. The authors emphasize a formal collaborative effort between cardiologists and cardiothoracic surgeons as the cornerstone for establishing a successful program, noting that a program without both specialties would be fundamentally deficient. Other factors on which success is based include ensuring patient safety and demonstrated commitment to excellence by the institution and procedural volume requirements.
The recommendations classify operating requirements for those that intend to develop a TAVR program, including credentialing requirements for cardiothoracic surgeons and interventional cardiologists who intend to perform the procedure, and guidance for maintaining approval to perform TAVR. Requirements include:
- Annual heart (aortic valve) surgery and percutaneous coronary intervention (PCI) volume requirements for institutions;
- Board certification and procedural requirements for both surgeons and interventional cardiologist;
- Monitoring of complication rates and institutional follow-up;
- Participation in a national registry that will include enrollment of all patients undergoing TAVR with continued tracking of outcomes; and
- Commitment to a heart team concept that is led by the surgeon and interventional cardiologist and made up of a formal collaborative effort among all medical team members. In all TAVR procedures, the interventional cardiologist and surgeon must both be present during the entire procedure ensuring joint participation and optimal patient-centered care.
"Maintaining high standards and a focus on quality improvement is at the core of what we do, for the sake of patients and their safety," said R. Morton Bolman, M.D., co-chair of the document writing committee, chief of the division of cardiac surgery at Brigham and Women's Hospital, and professor of surgery at Harvard Medical School. "This is emphasized in the paper released, as is the need for this to be a dynamic document that we will revisit in the future as the technology evolves, experience grows and data accumulate."
Watch the VIDEO “How to Build An Integrated Heart Team.” Brijeshwar Maini, M.D., and Brian Bethea, M.D., from Tenet Florida’s structural heart program, explain the importance of building a good heart team and how that team should interact.
For more information: www.scai.org, www.aats.org, www.cardiosource.org/ACC, www.sts.org


 December 24, 2025
December 24, 2025 









