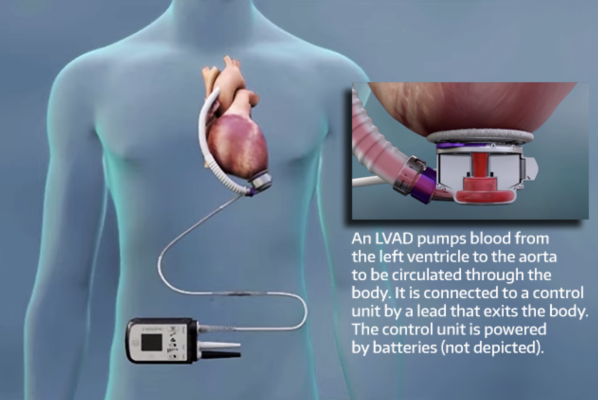
About one-fifth of implants of left ventricular-assist devices have the complication of right heart failure. Abbott Laboratories (adapted)
November 2, 2022 — For decades, left ventricular-assist devices (LVADs) have extended the lives of people whose hearts have grown too weak to effectively pump blood to the body. For upward of 20% of those patients, though, an LVAD implant gives rise to a dreaded complication: Their right ventricle fails, typically within days.
Cardiac specialists think it’s because the right heart cannot accommodate the suddenly resurgent blood flow from the just-installed pump. When right-heart failure is recognized, the patients receive intravenous medications and temporary mechanical support. In some cases, but not all, these emergency interventions improve the right ventricle’s viability.
Knowing beforehand which patients are at a higher risk to develop right-heart failure might enable doctors to reduce that likelihood.
Researchers at UW Medicine in Seattle today report findings of a machine-learning analysis of 186 pre-implant patient factors, revealing the 30 most strongly associated with right-heart failure among a population of 19,595 first-time LVAD recipients.
Their paper was published Oct. 26 in the ASAIO Journal.
“We had two objectives with this study: to help predict which patients will develop this complication and to find out if there are factors we can optimize to lower the risk of right-heart failure before we implant the LVAD,” said Dr. Song Li, a heart failure cardiologist at the UW Medicine Heart Institute and the paper’s senior author.
The sheer number of patient variables potentially involved in the complication has precluded cardiologists from easily knowing which ones, alone or in concert, might amplify risk for an LVAD recipient. Cardiologists have generally thought that the best predictor of right-heart failure post-LVAD implant is how the right heart functioned before surgery, Li said.
“We found that conventional wisdom might not be true: Right-heart function before LVAD is not one of the most important variables,” he said.
In this population, right-heart failure was most associated with patients’ liver function, kidney function, inflammation level, nutritional status, and overall preoperative acuity (INTERMACS profile), the authors found.
The puzzle of distinguishing variables’ relative importance was well-suited to an algorithm built to detect associations from a giant pool of data.
“Most traditional studies will come up with one risk factor that’s associated or correlated with an outcome. But for complex problems, it’s nice to be able to look at many variables at the same time,” said Dr. Arjun Bahl, the study’s lead author and a third-year resident in internal medicine.
The algorithm showed patient variables — for example, creatinine level, tobacco-smoking status and race — and their relative contributions to right-heart failure, Bahl said. The analysis also revealed whether a lower or higher variable value was more or less associated with the complication.
“Our machine-learning approach enabled us to move forward without having to create arbitrary cutoffs of levels to identify significance and without having to create subgroups of patients across those levels,” he said.
The researchers’ other consideration was to generate findings that are actionable for cardiologists.
“Now that we have a sense of what factors are more important, what can we do to optimize those before the patient goes into surgery?” Li asked. “Not all factors are modifiable, but for example nutritional status is one we could modify. We should try to give patients more nutrition, to ensure they are optimized before surgery.”
The researchers acknowledged that right-heart failure is not only dependent on presurgical patient factors, and that operative and postoperative care likely have an impact, as well.
For more information: http://www.uwmedicine.org/


 February 03, 2026
February 03, 2026 









