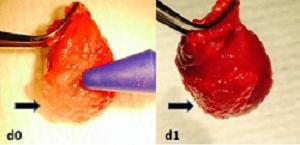
Hydrogel applied to beating rat hearts improves stem cell uptake by the heart muscle and speeds up tissue healing after heart attack. Image courtesy of Johns Hopkins Medicine.
September 29, 2015 — A sticky, protein-rich gel created by Johns Hopkins researchers appears to help stem cells stay on or in rat hearts and restore their metabolism after transplantation, improving cardiac function after simulated heart attacks, according to results of a new study.
The findings, described in the December 2015 issue of Biomaterials, offer a potential first step to a new way to heal human hearts after heart attacks as well.
The experiments build on the idea that although stem cells have shown enormous promise in repairing organs after injury, using them in the heart itself has not yielded the expected results because very few of the transplanted cells survive in the heart, said M. Roselle Abraham, M.B.B.S., M.D., assistant professor of medicine at the Johns Hopkins University School of Medicine and medical director of the Johns Hopkins Hypertrophic Cardiomyopathy Center of Excellence. When the heart beats, she explains, it pushes cells injected into the heart wall out into the lungs before they get a chance to attach to the wall.
Additionally, when stem cells move from the culture flasks they are grown in and into a solution for injection in the heart, their metabolism slows, causing them to die in several hours unless they are given the opportunity to attach to tissue.
Researchers have tried to improve stem cell retention in the heart by injecting millions, only to have a mere 10-20 percent stick around an hour after injection, Abraham said. And even then, she added, a large number of these cells die within 24 hours due to a sluggish metabolism.
“If we could inject fewer cells soon after heart attacks and coax them to proliferate following transplantation,” Abraham explained, “we could limit scar formation and be more successful with re-growing new heart muscle.”
In an effort to counter these difficulties, Abraham, along with then-Hopkins medical resident Angel Chan, M.D., Ph.D., joined forces with Jennifer Elisseeff, Ph.D., professor of biomedical engineering, ophthalmology and orthopedic surgery at the Johns Hopkins University School of Medicine and director of the Translational Tissue Engineering Center. Together, the researchers developed a hydrogel that combines serum, a protein-filled component of blood that contains everything cells need to survive, with hyaluronic acid, a molecule already present in the heart and in the matrix that surrounds and supports cells.
By mixing these two components, the researchers created a sticky gel that functioned as a synthetic stem cell niche: It encapsulated stem cells while nurturing them and rapidly restored their metabolism.
Tests in petri dishes showed that both adult and embryonic stem cells encapsulated in this material not only survived at levels near 100 percent but thrived for days and proliferated. The encapsulated cells also showed markedly higher production of growth factors known to be involved in cardiac repair compared with stem cells that weren’t encapsulated in the gel.
When the cell-gel combination was injected into living rat hearts, about 73 percent of the cells were retained in the hearts after an hour, compared with 12 percent of cells suspended in a solution. Over the next seven days, the number of regular solution-based transplanted cells continued to decline, whereas cells within the hydrogel increased in number.
In rat models of heart attack damage, moreover, Abraham’s team reports that the hydrogel with encapsulated cells improved pumping efficiency of the left ventricle over the four weeks after injection by 15 percent, compared with 8 percent from cells in solution. Even injections of the hydrogel on its own significantly improved heart function and increased the number of blood vessels in the region of the heart attack.
Chan, who is currently an advanced cardiac imaging and cardio-oncology fellow at Memorial Sloan Kettering, said that she chose this project because she was able to leverage her background in material science to design and fine tune the hydrogel for cardiac applications, and simultaneously obtain training in stem cell biology and multimodality molecular cardiac imaging. Her research experience inspired her to pursue advanced training in clinical cardiac imaging.
Other Johns Hopkins researchers involved in the study included Mehmet Karakas, Styliani Vakrou, Junaid Afzal, Andrew Rittenbach, Xiaoping Lin, Richard Wahl, Martin Pomper, Charles Steenbergen, Benjamin Tsui.
The work was funded by the American Heart Association grant AHABGIA and by the National Institutes of Health under grant numbers RO1 HL092985 and UL1 RR 025005.
For more information: www.hopkinsmedicine.org


 February 03, 2026
February 03, 2026 









