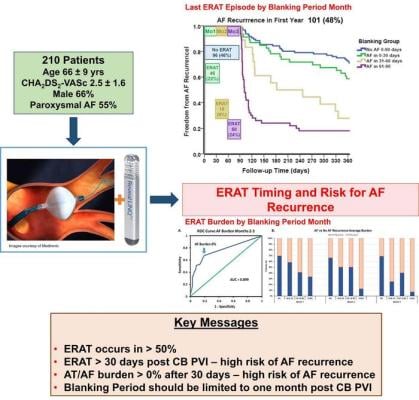
Based on continuous monitoring of early recurrence of atrial tachyarrhythmia immediately after patients have undergone atrial fibrillation ablation, Musat et al. recommend shortening the blanking period from three months to one. Graphic courtesy of Dan Musat
April 18, 2024 — New evidence-based research calls into question the conventional three-month blanking period immediately after atrial fibrillation (AF) ablation, when early occurrences of AF are thought not to predict long-term AF recurrence. Two articles and an accompanying editorial in Heart Rhythm, the official journal of the Heart Rhythm Society, the Cardiac Electrophysiology Society, and the Pediatric & Congenital Electrophysiology Society, published by Elsevier, address the controversy and recommend shortening the blanking period.
Early recurrence of atrial tachyarrhythmia (ERAT) is commonly seen following catheter ablation of AF, with reported incidences of up to 61% in the first three months. ERAT is often attributed to transient inflammation induced by tissue damage during ablation and short-term imbalances in autonomic innervation. This forms the physiologic rationale for the accepted convention of a three-month blanking period, during which arrhythmia recurrences are presumed to be relatively benign and not indicative of treatment failure. However, this reasoning disregards valuable data regarding early arrhythmia recurrences and their potential significance.
The authors of the editorial accompanying the two articles in Heart Rhythm call for the three-month blanking period to be reconsidered and posit that it might be time to "blank the blanking period" altogether. Lead author Jonathan M. Kalman, MBBS, PhD, from the Department of Cardiology, Royal Melbourne Hospital, Australia, says, "With increasing data indicating that early AF recurrence is a predictor of late recurrence, the three-month blanking period has been called into question. Although clinical trials assessing AF ablation have traditionally defined treatment success by the time to first AF recurrence, the use of such a binary efficacy outcome lacks clinical grounding and represents an oversimplification of the impact of ablative therapy."
Lead author of the article “Defining the blanking period, using continuous ECG monitoring, after cryoballoon pulmonary vein isolation,” Dan Musat, MD, from The Valley Hospital and The Snyder Center for Comprehensive Atrial Fibrillation, Ridgewood, NJ, USA, notes, "Multiple studies have challenged the duration of the blanking period. Our study used continuous monitoring and showed that both the timing of the last ERAT episode and the burden of ERAT show congruent results; any ERAT after the first month portends a worse outcome. Our data show that the ~1/3 of patients in whom ERAT occurs and/or have a burden of >0% after the first month post-cryoballoon pulmonary vein isolation, are at significantly higher risk of long-term recurrent AF. These findings lead us to consider changing the duration of the blanking period post-AF ablation to one month from the current three months."
Co-author Suneet Mittal, MD, from The Valley Hospital and The Snyder Center for Comprehensive Atrial Fibrillation, Ridgewood, NJ, USA, adds, “Our findings also demonstrate the value of continuous long-term ECG monitoring, because information about the presence and burden of AF can help inform clinical decision-making in patients following cryoballoon pulmonary vein isolation.”
In "Early atrial fibrillation recurrence post catheter ablation: Analysis from insertable cardiac monitor in the era of optimized radiofrequency ablation," De Becker et al. also emphasize the importance of continuous monitoring. They compiled data from Close-To-Cure and Close Maze studies, encompassing 165 patients who underwent radiofrequency (RF) ablation for paroxysmal or persistent AF. All patients were implanted with an insertable cardiac monitor two to three months before ablation. The study found that patients experiencing ERAT had a substantially higher risk of late recurrence, and the burden of ERAT during the blanking period was a significant predictor.
Lead investigator Benjamin De Becker, MD, from the Cardiology Department, AZ Sint Jan, Bruges, Belgium, explains, "During the blanking period, ERAT burden and ERAT occurring during the third month are independently associated with late recurrence. ERAT occurring after 64 days post-ablation was associated with a very high risk of late recurrence in both paroxysmal and persistent AF patients, suggesting that the conventional blanking period could be shortened. A blanking period post-AF ablation is mandatory to avoid unnecessary ablation because of procedural-induced arrhythmogenicity, and to avoid the occurrence of later repermeabilization of the RF lesions, which could require further reablation. Our research proposes that a two-month post-ablation blanking period would be an acceptable trade-off, minimizing the risk of an unnecessary repeat procedure. After this two-month period, atrial tachyarrhythmia occurrence is highly predictive of subsequent recurrences."
Professor Kalman concludes, "In light of this new evidence, a more stringent interpretation of these studies' findings might be that the very notion of a blanking period should be reconsidered. We believe that these data support a recommendation to eliminate the blanking period."
For more information: https://www.hrsonline.org/
Related content:
Novel Ablation Strategy Improves Freedom from Arrhythmias in Atrial Fibrillation Patients
Renal Artery Denervation and Catheter Ablation Increased Freedom From Atrial Fibrillation
VIDEO: New Approaches to Denervation Therapy
Renal Artery Denervation and Catheter Ablation Increased Freedom From Atrial Fibrillation
VIDEO: Device Therapies to Treat Hypertension
SPYRAL HTN-OFF MED Study Results Show Efficacy, Safety of Renal Denervation
Medtronic Announces Spyral HTN Global Clinical Trial Program for Renal Denervation
Medtronic Randomizes First Patients in Symplicity HTN-4
Medtronic Says its U.S. Renal Denervation Pivotal Trial Fails to Meet Primary Efficacy Endpoint
The Future of Renal Denervation Following the Failed SYMPLICITY HTN-3 Trial


 July 30, 2024
July 30, 2024