Results of the STROKE-VT trial showed direct oral anticoagulants (DOACs) are more effective than aspirin in reducing cerebrovascular events, including stroke in patients undergoing ventricular tachycardia ablation.
July 29, 2021 – Results of the STROKE-VT trial shows direct oral anticoagulants (DOACs) are more effective than aspirin in reducing cerebrovascular events, including transient ischemic attack and stroke in patients undergoing ventricular tachycardia using radiofrequency catheter ablation (RFA). The data were presented as a late-breaking clinical trial as part of Heart Rhythm 2021, the annual meeting for the Heart Rhythm Society (HRS).
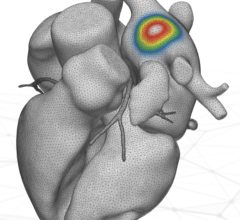
Catheter ablation is an established treatment for patients with atrial fibrillation (AF), the most common heart rhythm disorder. However, stroke and thromboembolism are known complications of left atrial (LA) catheter ablation, a procedure performed for those with symptomatic AF.[1] Left LA catheter ablation has a stroke risk of approximately 0.5 to 1%.[2] It has been shown within the electrophysiology (EP) field that when ablation procedures are conducted without anticoagulants (AC), patients are at an increased risk of stroke,[3] but the effect on anticoagulation for left ventricle procedures is understudied.
“The STROKE-VT trial helps us answer a longstanding question around the best way to lower procedure-related risks for patients coming out of an ablation,” said Dhanunjaya R. Lakkireddy, M.D., FHRS, executive medical director of the Kansas City Heart Rhythm Institute and lead author of the STROKE-VT study. “Moving forward, we hope the findings encourage electrophysiologists to use anticoagulants after ablations to reduce cerebrovascular events in a patient population that is already very sick and at high-risk of stroke.”
The study enrolled a total of 246 patients across four centers scheduled for left ventricular arrhythmia (LVA) RFA. Patients were randomized to receive either DOAC using apixaban (Eliquis) or aspirin (ASA) following their procedure which was then administered three hours after hemostasis. A brain MRI was conducted within 24 hours and at 30 days and neurological changes were assessed before, after, and at 30 days follow-up based on the National Institutes of Health NIH stroke scale.
Findings show significantly lower procedure-related complications in the DOAC arm than the ASA arm (3.7% vs. 24%; p<0.001). The rates of post-procedure cerebral vascular events (CVE) were lower in the DOAC arm compared to the ASA arm (4.5% vs. 19.6%, p<0.001 and 0 vs. 7.1%, p<0.001; respectively). At both 24 hours and 30 days, asymptomatic CVE on MRI were lower in the DOAC arm compared to the ASA arm (11.2% vs 25%, p=0.006 and 6% vs 19.6%, p=0.001; respectively).
The study was conducted at the Kansas City Heart Rhythm Institute in collaboration with Bristol-Myers Squibb.
Find additional HRS 2021 late breaking trials
Find more HRS 2021 conference news
References:


 July 30, 2024
July 30, 2024