October 31, 2011 — A panel presentation at the American College of Surgeons' annual clinical congress detailed how the contemporary practice of vascular surgery has evolved during the Iraq and Afghanistan wars. This has resulted in superior outcomes for complex, combat-related vascular injuries, including increased rates of amputation-free survival following extremity wounds.
The presentation, titled "Update on Wartime Vascular Injury and The Joint Theater Trauma Registry," was given by Lt. Col. Charles J. Fox, M.D., F.A.C.S., associate professor and past program director of vascular surgery at Walter Reed National Military Medical Center. It provided an overview of 10 years of vascular surgery advances in the current conflicts.
The presentation also highlighted the important role of the Joint Theater Trauma Registry (JTTR), a data collection tool created in 2004 as part of the Joint Theater Trauma System. The JTTR supports evidence-based improvements in battlefield trauma care, reduction of morbidity and mortality, and analysis of injury patterns, clinical decision-making and outcomes.
"Innovations in combat casualty care continue to advance the practice of both military and civilian vascular surgery," said Fox. "An important component is a multidisciplinary, team approach to treating patients with complex injuries."
Key innovations in caring for combat-related vascular injuries from the last decade include:
- Joint Theater Trauma System. This theater-wide trauma system was established in conjunction with the U.S. Army Institute of Surgical Research and the American College of Surgeons Committee on Trauma. It led to deployment of forward surgical teams with Level III capabilities much closer to soldiers in the field. Surgeons now definitively repair all recognized vascular injuries before soldiers leave Iraq or Afghanistan. Fast evacuation is possible with a median time of approximately 8.5 days from the point of vascular injury in theater to arrival in a United States level V facility. Weekly teleconferences across three continents take place to discuss ongoing management of vascular injuries; in addition, Web-based electronic medical records that follow soldiers back home, ensuring continuity of care.
- Widespread use of tourniquets. In a reversal of previous medical practice, the military now widely distributes tourniquets and trains soldiers and medics in their use. Most combat-related extremity injuries now arrive with tourniquets applied pre-hospital; the practice is widely credited with saving the lives of soldiers who might have died on the battlefield in previous conflicts due to hemorrhage.
- Advances in damage control resuscitation (DCR). DCR techniques, such as rapid transfusion of fresh, warm blood components and treating hypothermia upon admission to battlefield hospitals, enable vascular surgeons to perform more procedures in forward deployed (Level III) surgical sites closer to the fight; this avoids delaying treatment waiting to evacuate patients to higher-level trauma hospitals. Modern DCR practices helped reduce case fatality rates to 9.4 percent in the current conflicts compared to 19.1 percent in World War II and 15.8 percent in Vietnam.
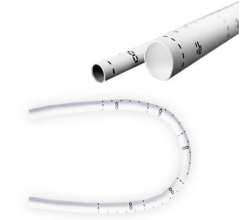
- Temporary vascular shunts. These devices give military surgeons additional time to address more life-threatening injuries, assess treatment options and, if needed, evacuate soldiers from battlefield hospitals.
The U.S. Army continues to examine clinical outcomes and JTTR data in its quest to enhance battlefield care. Fox described areas for future research and emerging endovascular therapies to further improve the diagnosis and treatment of combat-related vascular injuries. For example, the availability of advanced diagnostic imaging equipment, such as CT scanners, as well as modern catheters and stents, increases the variety and complexity of endovascular interventions possible at Level III battlefield hospitals.
These less-invasive technologies also allow surgeons to find and address hidden vascular injuries that may otherwise have gone unnoticed for weeks.
The Army has also promoted the widespread use of closed negative pressure wound therapy. The technique enables surgeons to close deep soft tissue wounds, typically caused by explosions, to ensure vessel grafts remain covered with healthy muscle tissue. This emerging therapy is improving surgeons' ability to close large cavity wounds that previously would have required amputation.
Graft surveillance provides useful clinical data to generate modern guidelines for emergent limb reconstruction in the repair of combat-related vascular injuries. An ultrasound offers a less invasive alternative to angiography and catheter-based arteriograms that are usually performed at the time of injury or shortly after evacuation.
Vascular injuries comprise up to nine percent of combat-related injuries sustained in Iraq and Afghanistan, triple the rate during Vietnam; extremity injuries account for 75 percent of all vascular injuries in the current conflicts. Analysis of vascular injury patterns, vessel repair methods and patient outcomes based on JTTR data led to improvements in soldier training, equipment and combat casualty care over the last decade. This has allowed a greater percentage of soldiers suffering vascular trauma to survive long enough to reach medical care.
The panel presentation was based on the article, "Update on Wartime Vascular Injury," by Lt. Col. Fox, Bhavin Patel, B.S., and Lt. Col. W. Darrin Clouse, M.D., F.A.C.S., published in the March 2011 issue of the journal Perspectives in Vascular Surgery and Endovascular Therapy.
For more information: www.healthcare.goarmy.com


 February 06, 2026
February 06, 2026