Getty Images
December 18, 2023 — An artificial intelligence (AI) tool developed by investigators at the Smidt Heart Institute at Cedars-Sinai and colleagues at two other institutions accurately predicted how patients would fare after cardiac surgeries and procedures.
The results, published in The Lancet Digital Health, include data from patients from three healthcare systems: Cedars-Sinai, Stanford University and Columbia University. All patients in the study underwent a surgical procedure, including open heart surgery, other major surgeries, and minimally invasive procedures involving a catheter or endoscope.
Investigators trained an AI model on pre-operative electrocardiograms, discovering a new use for the 130-year-old test. Invented in the late-1800s, an electrocardiogram is a commonly deployed test that involves placing electrodes on the skin to measure the heart’s electrical activity and assess how well the heart is functioning.

“This is the first electrocardiogram-based AI algorithm that predicts post-operative mortality,” said David Ouyang, MD, a cardiologist in the Department of Cardiology in the Smidt Heart Institute at Cedars-Sinai, and a corresponding author of the study. “Previously, algorithms have been used to assess long-term mortality as well as individual disease states, but determining post-surgical outcomes helps inform the actual decision to do surgery.”
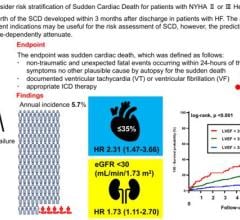
While classifying most patients as low risk, those individuals the algorithm identified as high risk had nearly a 9-fold increased probability of post-operative mortality.
“As it now stands, clinicians only have a modest ability to predict how a patient is going to do after surgery,” said Ouyang, also a faculty member in the Division of Artificial Intelligence in Medicine at Cedars-Sinai. “Current clinical risk prediction tools are insufficient. This AI model could potentially be used to determine exactly which patients should undergo an intervention and which patients might be too sick.”
“In cardiology, we're fortunate to have many life-saving procedures, everything from catheter-based procedures to open-heart surgery, so we're often trying to think about who are the right patients for the right procedure,” said Christine M. Albert, MD, MPH, chair of the Department of Cardiology in the Smidt Heart Institute and the other corresponding author of the study. “A better understanding of risk, particularly by using a commonly obtained diagnostic test, can inform important medical decisions.”
Investigators are currently studying how the algorithm could be translated into a web application that would be widely available for physicians and patients.
For more information: www.cedars-sinai.org



 October 02, 2024
October 02, 2024