Amanda and her husband, Nathan, doting on their daughter, Kassidy, minutes after her arrival.
April 23, 2014 — Three weeks after delivering her first child, Amanda began to suffer from extreme fatigue, headaches, a tight chest and stomach pain. An initial diagnosis of pneumonia changed for the worse: Amanda was experiencing heart failure. The 28-year-old’s life was at risk. She was quickly transferred to UC San Diego Sulpizio Cardiovascular Center (SCVC) where a multidisciplinary team implanted a novel cardiac device under her skin, leaving the heart untouched, to prevent sudden cardiac arrest.
“When Amanda first arrived at SCVC, she was in critical condition. It became clear within 24 hours that she needed emergency surgery or she would not survive,” said Eric Adler, M.D., director of cardiac transplant and mechanical circulatory support at UC San Diego Health System.
The new mother was diagnosed with peripartum cardiomyopathy, a rare disorder in which a woman develops heart disease within the final month of pregnancy or within five months after delivery. Adler added that one in 2,000 women suffers from the condition, the cause is not exactly known and it can be hard to correctly diagnosis.
“I knew I had to fight for my daughter,” said Amanda. “I am not a quitter and always strive for success. I wasn’t going to let heart failure beat me.”
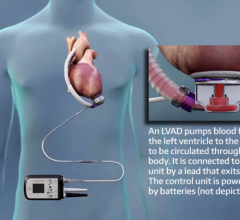
A left ventricular assist device (LVAD) — a mechanical heart of sorts that helps pump oxygen-rich blood throughout the body — was first implanted in Amanda.
“The patient’s heart was failing. She was in a dire situation and needed the LVAD device immediately implanted to support her heart function and restore blood circulation,” said Victor Pretorius, MBchB, cardiothoracic surgeon at UC San Diego Health System, who implanted the LVAD in Amanda.
Amanda was also a candidate for the new Boston Scientific Subcutaneous Implantable Cardioverter Defibrillator (S-ICD) System. The device is used for the treatment of patients at risk for sudden cardiac arrest. To date, more than 3,000 devices have been implanted in patients around the world.
The S-ICD System monitors cardiac activity and shocks the heart when it goes into a dangerous rhythm, a function not performed by the LVAD. The S-ICD does not use traditional wires, called “leads,” threaded to the heart through blood vessels. Rather, the device is implanted just under the skin near the breastbone, and heart patients who require an ICD may be candidates.
“Leads in standard ICDs have been known to fracture or disconnect at times. The S-ICD has fewer long-term complications, an easier removal process and puts the patient at less risk for infection,” said Ulrika Birgersdotter-Green, M.D., director of pacemaker and ICD services at UC San Diego Health System, who implanted the device in Amanda. “It is an advancement in defibrillation technology that is simple to implant and can be life-saving.”
Amanda was the first patient at UC San Diego Health System to receive the S-ICD. The procedure took about an hour, and she was able to walk around the next day. As she continues to heal, she will be closely monitored to see if her heart function improves. If not, she will be placed on a heart transplant list.
“As part of the region’s only academic hospital, we are dedicated to using a team approach to treat high risk patients, who five to ten years ago, may not have survived,” said Adler.
Amanda is now sharing her story to raise awareness about heart disease.
“Knowledge and early detection for heart disease, especially peripartum cardiomyopathy, are key. I hope my story helps others to understand the warning signs and the technology available for treatment,” said Amanda. “The first time I was able to hold my daughter after the procedure, I became very emotional after the journey I had just been through. Because of the team at SCVC, I am able to embrace my family every day.”
For more information: heart.ucsd.edu


 June 19, 2024
June 19, 2024