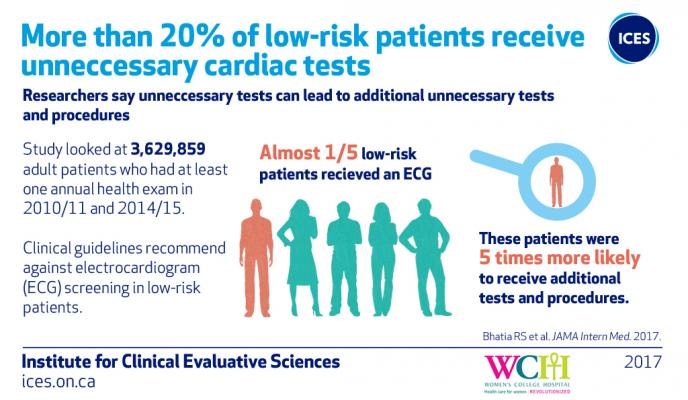
July 20, 2017 — More than one in five Ontario patients receive an electrocardiogram (ECG) during their annual health exam despite being at low risk for heart disease, according to a new study from the Institute for Clinical Evaluative Sciences (ICES).
An ECG is a common test used to record the electrical signals of the heart; the results of an ECG can provide information about the structure and function of the heart.
“An ECG is a valuable test that can save a patient’s life if they are experiencing chest pains or are at high risk of heart disease, but there is little value when patients are at low risk of cardiovascular disease and this certainly should not be a routine test as part of an annual physical exam,” said Sacha Bhatia, M.D., a scientist at ICES, cardiologist and director at Women’s College Hospital Institute for Health System Solutions and Virtual Care (WIHV).
The study, published in JAMA Internal Medicine, shows that low-risk patients who had an ECG were five times more likely to receive another diagnostic test like a stress test, echocardiogram or a cardiology consultation than those who did not have an ECG.
“Our findings show that ECGs conducted on patients as part of an annual health exam are common, and the downstream effect is an increased risk for subsequent cardiology testing and consultation cascade, even though the overall cardiac event rate in this group was very low,” added Bhatia.
The Choosing Wisely campaign, launched in 2012, recommends against non-invasive cardiac testing in low-risk and asymptomatic patients. ECGs are in their “top five” lists of low-value tests, treatments and procedures that physicians and patients should question.
The study of 3,629,859 adult patients who had at least one annual health exam between fiscal years 2010/2011 and 2014/2015 in Ontario found:
- ECGs ordered in low-risk patients as part of the annual health exam are common, occurring in 21 percent of patients;
- There is wide variation in physician ordering, with more than 7 percent of family physicians ordering ECGs in more than 50 percent of their low-risk patients;
- In low-risk patients who had an ECG, they were five times more likely to receive another test (like a stress test, echocardiogram) or cardiology consultation than those who did not; and
- Patients that did or did not receive an ECG had a very low risk of death, hospitalizations or revascularization (<0.5 per cent) at the one-year mark.
“Our findings suggest that even low-cost procedures like ECGs in low-risk patients, occur with significant frequency, and importantly can lead to more advanced testing that ends up costing the health system more with little potential benefit to patients,” said Bhatia.
For more information: www.jamanetwork.com/journals/jamainternalmedicine


 November 12, 2025
November 12, 2025 









