October 23, 2019 — Proactive administration of amiodarone to patients recovering from a common heart surgery shows promise in preventing postoperative atrial fibrillation, a serious and expensive complication with potential long-term consequences.
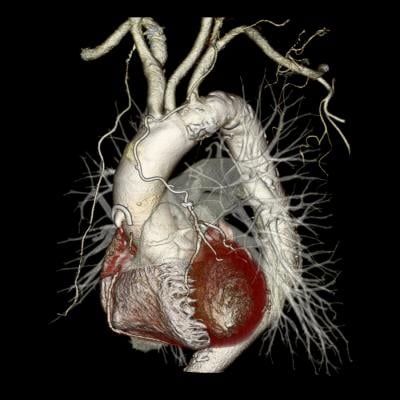
“Reducing New-Onset Atrial Fibrillation After Coronary Artery Bypass Graft Surgery” discusses how Beaumont Hospital, Dearborn, Mich., developed and implemented an evidence-based protocol to use amiodarone as a prophylaxis after coronary artery bypass graft (CABG) surgery. The article is published in AACN Advanced Critical Care.[1]
The quality improvement project resulted in a decreased incidence of postoperative atrial fibrillation (POAF) (17 percent versus 25 percent) and shorter mean lengths of stay. The results indicate that the protocol could significantly reduce costs, improve patient outcomes and increase the overall quality of care.
POAF is the most common dysrhythmia to occur after CABG surgery, affecting 10-40 percent of patients. At Beaumont, nearly a quarter of patients with CABG developed POAF in 2016 and during a six-month period in 2017, establishing a baseline for the study.
Co-author Melanie Coletta, DNP, CCRN, AGACNP-BC, is a cardiothoracic nurse practitioner at the hospital. The multidisciplinary research team also included the chief of cardiac and thoracic surgery and a cardiology clinical pharmacist specialist, as well as faculty from the nurse practitioner program at the College of Nursing and Health at nearby Madonna University.
“Prior to the protocol, we administered amiodarone reactively to treat POAF, rather than proactively to prevent it,” she said. “We’re continuing to assess and adjust the protocol to improve patient outcomes and generate additional data to support a potential clinical practice guideline specific to the prevention of POAF in the cardiac surgical patient population.”
After an extensive literature review, the research team collaborated to develop an amiodarone POAF prophylaxis protocol, including determining which patients met the inclusion criteria, medication administration and dosing strategy. An order set for the protocol was then created and embedded into the electronic health record as part of the cardiac surgery postoperative order set.
A total of 68 CABG surgeries were performed from Nov. 1, 2017, to Feb. 15, 2018. After exclusions, 47 patients completed the protocol and were included in the statistical analysis.
Eight of the patients receiving amiodarone prophylaxis (17 percent) developed POAF, and none of them were readmitted with dysrhythmia within 30 days of discharge. In addition, the mean length of stay for the entire study group was six days, which falls within the CABG reimbursement time frame of seven days. In the 2017 baseline group, the mean length of stay was seven days for patients without POAF and eight days for those who developed it.
The article is part of a symposium published in the fall 2019 issue of the peer-reviewed journal that focuses on the positives and negatives of medications in critical care.
Mary Fran Tracy, Ph.D., RN, APRN, CCNS, served as editor for the symposium. She is associate professor, University of Minnesota (UM) School of Nursing, and nurse scientist at UM Medical Center.
“Medications are powerful tools in the arsenal for patient care, especially in critical care, but they can be both friend and foe,” she said. “We are gaining ever-advancing knowledge related to new and traditional drugs, as well as increased understanding of how individuals respond to medications with both appropriate and illicit use.”
For more information: www.acc.aacnjournals.org
Reference
1. Coletta M.J., Lis G., Clark P., et al. Reducing New-Onset Atrial Fibrillation After Coronary Artery Bypass Graft Surgery. AACN Advanced Critical Care, published online Fall 2019. doi: 10.4037/aacnacc2019470


 December 19, 2025
December 19, 2025 









