May 18, 2018 — Data on the effectiveness of cardiac resynchronization therapy (CRT) in patients with non-left bundle branch block (non-LBBB) is limited and when available has been shown to be suboptimal compared to LBBB patients. A new study presented at the 2018 Heart Rhythm Society (HRS) Scientific Sessions, May 9-12 in Boston, compared the effects of targeting the region of increased electrical delay (QLV approach) for left ventricular (LV) lead location to a standard of care (SOC) anatomical implant approach in non-LBBB patients. The comparison was assessed on the Clinical Composite Score (CCS) after 12 months of follow-up.
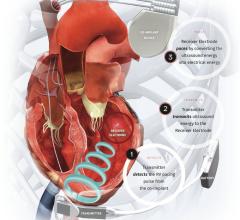
CRT is usually delivered through an anatomical implant approach placing the left ventricular (LV) lead in the mid-lateral or posterolateral wall. Since the left ventricular activation sequence in non-LBBB patients is different from that in LBBB, it was postulated that targeting the region of increased electrical delay (QLV approach), may serve as a more individualized strategy in this cohort of patients.
A total of 248 patients were enrolled in the ENHANCE CRT Pilot Study at 29 U.S. centers. Following enrollment, patients were randomized in a 2:1 ratio between a QLV-based implant (QLV arm) and SOC anatomical implant approach (SOC arm) and implanted with a St. Jude Medical quadripolar CRT-D system per the 2013 ACCF/AHA/HRS guidelines. The primary endpoint was the CCS (NYHA class, Patient Global Assessment, heart failure events and cardiovascular death) after 12 months of follow-up.
A total of 190 subjects were available for data analysis at 12 months of follow-up (128 QLV arm; 62 SOC arm). Of these, 39 subjects had worsening heart failure events (8 cardiac deaths and 31 heart failure hospitalizations), 26 in the QLV arm and 13 in the SOC arm. There were no differences in baseline characteristics between the QLV and SOC arms. The CCS responder rate at 12 months of follow-up was 63.7 percent in the QLV arm and 71.4 percent in the SOC arm (p=0.388). Subjects demonstrated a statistically significant improvement in MLWHF score from baseline to 6 months and to 12 months in the SOC arm (18.4 ± 23.3 and 15.1 ± 20.9) and in the QLV arm (17.6 ± 27.6 and 17.0 ± 26.0) (all p<0.001). There were statistically significant increases in left ventricular ejection fraction (LVEF) from baseline to 6 and to 12 months for the SOC arm (5.0 ± 8.4% and 5.5 ± 11.0 %) and for the QLV arm (5.5 ± 11.0 % and 5.8 ± 9.6 %) (all p<0.001). There were no significant differences between the two interventional arms in quality of life or LVEF.
CRT in non-LBBB patients was associated with a marked clinical improvement as evidenced by the CCS and favorable reverse remodeling. However, there was no difference in the outcome of patients between the QLV arm versus the SOC anatomical left ventricular lead implantation arm. Further analysis pertinent to the interactions between the QLV strategy and final anatomical lead locations along with updated results were presented at the HRS meeting.
For more information: www.hrssessions.org
Related HRS Content
Heart Rhythm 2018 Late-breaking Studies


 July 21, 2025
July 21, 2025