April 25, 2025 – Findings from two late-breaking clinical trials demonstrate the safety and efficacy of left bundle branch area pacing (LBBAP), adding to the growing body of evidence supporting new pacing methods. Researchers presented these findings as late-breaking clinical science during Heart Rhythm 2025.
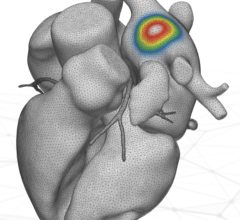
Heart failure impacts more than 64 million people worldwide.1 While numerous studies have shown that cardiac resynchronization therapy (CRT) can reduce hospitalizations related to heart failure and lower allcause mortality, biventricular pacing (BVP) has notable limitations, including a 3–4% rate of acute procedural failure, phrenic nerve stimulation, and increasing pacing thresholds or loss of capture.2 LBBAP continues to gain attention as a promising pacing option in patients with more complex conduction system diseases, particularly for patients with infranodal atrioventricular block and left bundle branch block.3
The findings of the following studies contribute to the expansion of treatment capabilities using LBBAP.
Left Bundle Branch Area Pacing for Cardiac Resynchronization Therapy
I-CLAS, a global, multicenter registry, compared the clinical outcomes between BVP and LBBAP among patients with left ventricular ejection fraction (LVEF) <50% undergoing CRT. The study included 2,579 patients from 18 international centers. At a mean follow-up of 34±15 months, the results showed that LBBAP was associated with significantly better outcomes compared to BVP, including a lower rate of death or heart failure hospitalization (22.2% vs. 30.8%), and reduced time to heart failure hospitalization (13.6% vs. 20.8%).
“Our findings support the hypothesis that targeting the conduction system through left bundle branch area pacing leads to superior electrical resynchronization, resulting in better clinical outcomes,” said Pugazhendhi Vijayaraman, MD, Director of Cardiac Electrophysiology, Geisinger Heart Institute, WilkesBarre, Pennsylvania. “While these results are promising, ongoing large randomized controlled trials will offer further insights into the long-term benefits of left bundle branch area pacing.”
Small-Diameter Defibrillation Lead Effectiveness
When Placed in the Left Bundle Branch Area The LEADR LBBAP study, a global, prospective, non-randomized, multi-center study, sought to evaluate the safety and efficacy of the OmniaSecure™ defibrillation lead when placed in the LBBAP position. The OmniaSecure lead demonstrated high defibrillation success in LBBAP for patients indicated for an ICD or CRT-D. The study met its prespecified efficacy goal of 88% and defibrillation was 100% successful following testing conducted at device implantation in 162 patients. These results demonstrate the potential for the OmniaSecure defibrillation lead to be used in alternative areas other than right ventricular stimulation for sensing, pacing, cardioversion, and defibrillation.
“For the first time, we are seeing promising evidence that this novel lead can be used in alternative locations, allowing physicians to place the lead in the optimal position for each patient, ultimately enhancing the precision of treatment. The positive defibrillation results are encouraging and highlight the potential versatility of the OmniaSecure lead,” said Dr. Vijayaraman. “Future analyses will provide further insights into the safety and efficacy of the lead at 3-months follow-up.”
For more information, visit www.HRSonline.org.
- Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GMC, Coats AJS. Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res. 2023; 118(17):3272-3287.
- Diaz JC, Duque M, Aristizabal J, Marin J, Niño C, Bastidas O, Ruiz LM, Matos CD, Hoyos C, Hincapie D, Velasco A. The emerging role of left bundle branch area pacing for cardiac resynchronisation therapy. Arrhythmia & Electrophysiology Review. 2023; 12: e29.
- Huang W, Zhou X, Ellenbogen KA. Pursue physiological pacing therapy: a better understanding of left bundle branch pacing and left ventricular septal myocardial pacing. Heart Rhythm. 2021; 18(8):1290-1.


 July 30, 2024
July 30, 2024