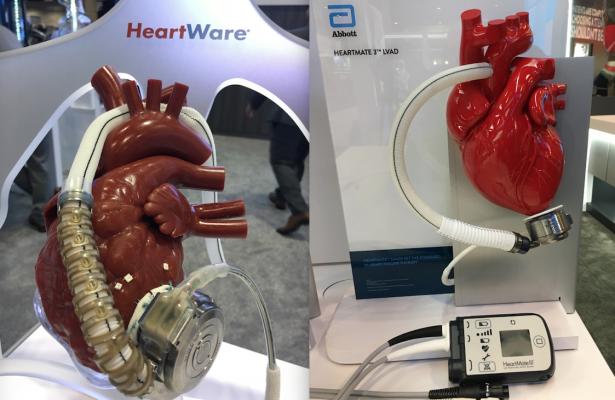
CMS coverage changes effective as of Dec. 2, 2020 will open up the use of LVADs to more Medicare patients, including use of the HeartWare and HeartMate ventricular assist devices.
December 2, 2020 — The Centers for Medicare and Medicaid Services (CMS) finalized updates to Medicare coverage policies for artificial hearts and ventricular assist devices (VADs) to treat patients with advanced heart failure.
While Medicare generally does not cover experimental or investigational items and services, the program has historically allowed for coverage of certain interventions when they are provided in the context of an approved clinical study or with the collection of additional clinical data. This process can allow for earlier beneficiary access to innovative treatments and technology while additional data is collected.
Prior to today, Medicare covered artificial hearts under this “coverage with evidence development” standard. The updated coverage policy CMS is announcing today will end this requirement for artificial hearts and instead allow for the more standard coverage determination process where coverage decisions are made by local Medicare Administrative Contractors (MACs).
CMS said it believes this final decision is in the best interest of Medicare beneficiaries since careful patient selection is important, and the MACs are structured to take into account a beneficiary’s particular clinical circumstances to determine which patients will benefit from receiving an artificial heart. Although a small number of Medicare beneficiaries receive artificial hearts, the technology can save the lives of certain end-stage heart failure patients awaiting heart transplantation.
“CMS is dedicated to improving cardiovascular health in the Medicare population,” said CMS Administrator Seema Verma. “CMS is continually updating our policies to ensure that Medicare beneficiaries have access to the latest technology and appropriate evidence-based healthcare. These coverage changes will give beneficiaries and providers more options as they choose the potentially life-saving treatments most likely to produce good health outcomes.”
The final national coverage determination, which is effective as of December 2, 2020, also provides updated coverage criteria for VADs that better aligns with current medical practice and that we believe will expand coverage to a greater number of candidates who are likely to benefit from this technology. Specifically, the updated patient criteria in the NCD aligns with the inclusion criteria derived from recent large randomized controlled trials, which demonstrated improved patient outcomes.
New CMS Coverage Policy for Ventricular Assist Devices
The decision is limited to durable, intracorporeal, left ventricular assist devices (LVADs), and does not include temporary VADs or extracorporeal membrane oxygen (ECMO). CMS is establishing coverage according to the following conditions:
• Removes the current therapeutic intent-to-treat criteria of bridge-to-transplant (BTT) and destination therapy (DT), by removing the following BTT requirements:
• The requirement that the patient is active on the waitlist maintained by the Organ Procurement and Transplantation Network (OPTN).
• The requirement that the implanting site, if different than the Medicare-approved transplant center, must receive written permission from the Medicare-approved transplant center prior to implantation of the VAD.
• Extends evidence based patient selection criteria, that previously applied only to DT, for all LVAD procedures for short-term (e.g., bridge-to-recovery and bridge-to-transplant) or long-term (e.g., destination therapy) mechanical circulatory support (see below in covered indications).
• Modifies patient selection criteria to reflect the major inclusion criteria of contemporary trials.
CMS Covered Indications For LVADS
Left ventricular assist devices are covered if they are FDA-approved for short-term (e.g., bridge-to-recovery and bridge-to-transplant) or long-term (e.g., destination therapy) mechanical circulatory support for heart failure patients who meet the following criteria:
• Have New York Heart Association (NYHA) Class IV heart failure; and
• Have a left ventricular ejection fraction (LVEF) ≤ 25%; and
• Are inotrope dependent - OR - have a cardiac index (CI) < 2.2 L/min/m2, while not on inotropes, and also meet one of the following:
A. Are on optimal medical management (OMM), based on current heart failure practice guidelines for at least 45 out of the last 60 days and are failing to respond; or
B. Have advanced heart failure for at least 14 days and are dependent on an intra‐aortic balloon pump (IABP) or similar temporary mechanical circulatory support for at least 7 days.
• Beneficiaries receiving a VAD must be managed by an explicitly identified, cohesive, multidisciplinary team of medical professionals with appropriate qualifications, training, and experience. The team embodies collaboration and dedication across medical specialties to offer optimal patient-centered care. Collectively, the team must ensure that patients and caregivers have the knowledge and support necessary to participate in informed decision making. The team members must be based at the facility and must include individuals with experience working with patients before and after placement of a VAD.
To read the final CMS decision at: https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=298&type=Closed&bc=AIgAAAAACAAA&


 May 30, 2025
May 30, 2025 









