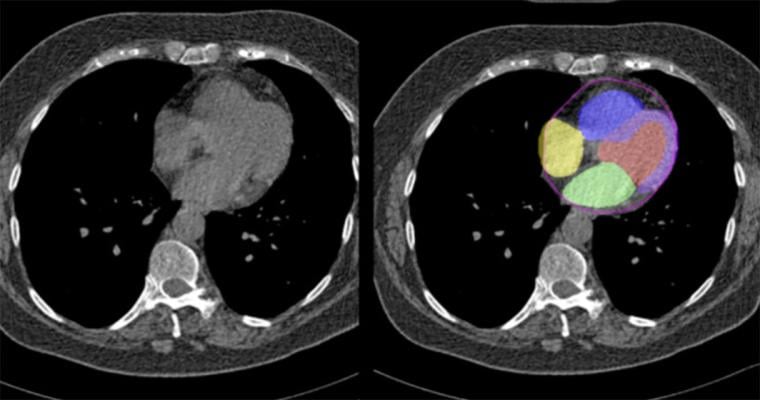
Cedars-Sinai investigators can identify comprehensive cardiovascular risk from CT scans obtained without contrast dye, which some patients cannot tolerate, through the use of AI algorithms. Image by Cedars-Sinai.
April 23, 2024 — A recent study designed and implemented by investigators at Cedars-Sinai found that artificial intelligence (AI) can accurately evaluate cardiovascular risk during a routine chest computed tomography (CT) scan without contrast. This imaging method, which measures coronary calcium and sizes of heart chambers and heart muscle, could make identifying cardiovascular risk less expensive and less invasive.
The findings were published in the peer-reviewed journal Nature Communications.
A recent study designed and implemented by investigators at Cedars-Sinai found that artificial intelligence (AI) can accurately evaluate cardiovascular risk during a routine chest computed tomography (CT) scan without contrast. This imaging method, which measures coronary calcium and sizes of heart chambers and heart muscle, could make identifying cardiovascular risk less expensive and less invasive.
The findings were published in the peer-reviewed journal Nature Communications.
“These results are likely practice-changing for many patients because this technology can accurately identify cardiovascular risk without the use of invasive tests or contrast dye that some patients cannot receive,” said Piotr J. Slomka, PhD, director of Innovation in Imaging at Cedars-Sinai, professor of Medicine in the Division of Artificial Intelligence in Medicine and senior author of the study.
Slomka, a professor of Cardiology in the Department of Cardiology in the Smidt Heart Institute at Cedars-Sinai, said that more than 15 million CT scans are performed in the U.S. each year--and many of these are underutilized or understudied. Clinicians currently can evaluate cardiovascular risk using a CT scan, but usually with contrast.
“This novel AI algorithm makes it possible to get crucial heart health insights from cheaper scans that use less radiation, potentially making detailed heart evaluations part of regular diagnostic procedures,” Slomka said.
Investigators incorporated two artificial intelligence models to evaluate data on coronary calcium and heart muscle chamber sizes from nearly 30,000 patient imaging records. They were able to determine that those measures are a better indicator of cardiac risk than a radiologist’s identification of abnormalities.
Sumeet Chugh, MD, director of the Division of Artificial Intelligence in Medicine, who was not involved in the study, says this technology allows for large-scale use of existing CT data to spot individuals at risk sooner.
“Coronary artery disease is the leading cause of disability and death at a global level,” said Chugh, associate director of the Smidt Heart Institute. “These findings highlight how AI tools could leverage existing CT images performed for lung disease investigation, to make a cost-effective, public health impact on heart disease.”
The collective group of Cedars-Sinai investigators that developed these findings also included teams from the Smidt Heart Institute, the Biomedical Imaging Research Institute and the Department of Biomedical Sciences.
Other Cedars-Sinai authors include Robert J. H. Miller, Aditya Killekar, Aakash Shanbhag, Bryan Bednarski, Anna M. Michalowska, Mark Lemley, Konrad Pieszko, Serge D. Van Kriekinge, Paul B. Kavanagh, Joanna X. Liang, Cathleen Huang, Damini Dey and Daniel S. Berman. Other investigators include Terrence D. Ruddy, Andrew J. Einstein and David E. Newby.
This research was supported in part by grant R35HL161195 from the National Heart, Lung, and Blood Institute/National Institutes of Health (NHLBI/NIH) (PI: PS) as well as R01EB034586 from the National Institute of Biomedical Imaging and Bioengineering (PI: PS). The authors thank the National Cancer Institute for access to NCI’s data collected by the National Lung Screening Trial (NLST) accessed under project number NLST-981. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
For more information: www.cedars-sinai.org


 February 03, 2026
February 03, 2026 









