The Impella 2.5 Cardiac Assist Device by Abiomed pumps up to 2.5 liters of blood per minute.
Physicians recognize the importance of ventricular assist devices (VADs) every time a congestive heart failure (CHF) patient awaiting transplantation gets a therapeutic bridge. But VADs are playing an increasingly critical role not just in improving patient outcomes but also in cutting overall healthcare costs.
With the recent introduction of new VAD models and upgrades in the U.S., in addition to new devices entering final clinical trials this year, these technological innovations promise to further bridge the gaps in both patient care and healthy healthcare spend.
New Hope for CHF
CHF is a chronic condition associated with damage that results in insufficient functioning of the heart. Currently, the U.S. has five million patients suffering from CHF with an estimated 550,000 patients being diagnosed every year. In the treatment of CHF, VADs play a vital role in the continuum of care, which includes pharmacotherapy and heart transplantation.
Augmenting the demand for VADs is the mounting shortage of organ donors, illustrated by the fact that in 2006 only 2,192 actual implants were performed against a potential demand of 40,000. In 2007, the heart transplant waiting list had 2,723 patients.
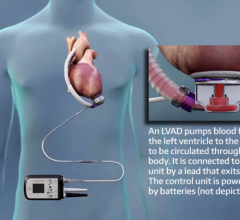
The utility of VADs cannot be underestimated as it provides immediate hemodynamic support and a new lease on life for critically ill patients. Initially developed as a last resort temporary bridge to transplant, with new developments in VAD technology and the overwhelming successful outcomes witnessed in certain patients, device developers have begun to realize that their potential is much more. VADs are now seeking to be used in destination therapy where patients are unfit to undergo a transplant. These powerful devices, also used as a bridge to recovery, provide post-cardiotomy support to patients who cannot be weaned off a heart-lung machine. Hence VADs have demonstrated a great deal of versatility with proven applications in long–term, intermediate and short-term care.
Complications associated with VAD support include hemolysis, infection, bleeding, thromboembolism and device- related failure. Success with VAD support largely depends on patient selection. Surfaces within the device that come in contact with blood are extremely smooth and are coated with heparin to prevent thromboembolism and also promote flow characteristics. Complication rates are expected to decrease as experience and device design improvement reach a level of competence. Incidence of complications is likely high in long-term VAD support where mortality is largely attributed to device malfunction. In the short-term, support mortality is related to bleeding, infection and multi-organ failure.
VADs were originally developed for long-term therapy. However, their success pertaining to VAD support as bridge to transplant has extended their application as long-term destination therapy. The survival rates of using VADs as a bridge to transplant have been established as 84 percent, 74 percent, 64 percent and 55 percent at 30 days, three months, 1 year and four years. However, the adoption of VADs as a permanent transplant is pretty recent and has not been very aggressive, with the INTrEPID (Investigation of Non-Transplant Eligible Patients who are Inotrope Dependent) and REMATCH (Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure) trials yielding survival rates of 27 percent and 52 percent respectively. In 2003, the FDA approved the HeartMate XVE for destination therapy. A lot more will need to be done in terms of device design and patient selection to improve clinical outcomes in destination therapy where VADs can be used on a wide range of patients.
VADs have had a great impact in helping the older patients (>60 years) travel to see the world and enjoy a relatively active life. These lifesaving devices have also helped the younger patients (20 to 60 years) live longer and productive lives.
Cutting Complications, Cost
In 2008, heart failure has thus far been associated with direct and indirect healthcare costs of an estimated $34.8 billion. These numbers have urged overall the healthcare industry to channel its focus toward cutting costs, and VADs are devices that virtually pay off in this direction. Costs for the new dimension of outpatient therapy with VADs are estimated at $13,200 versus inpatient costs of $165,200 with just room and board. Some of the devices that facilitate outpatient therapy include the HeartMate vented electric left ventricular assist system (LVAS) and the Novacor LVAS. These devices are implanted within the thoracic and abdominal cavity and are connected to the power source through a percutaneous driveline.
Life after VAD transplantation has often resulted in making patients less dependent to perform their daily activities, and has even helped some patients get back to work. Subsequently reimbursements for implanting VADs have been encouraging, averaging around $130,000 and $140,000.
New Devices Flood the Market
The global market for VADs in 2008 accounts to an estimated $233 million, and is expected to continue to grow. However, widespread adoption of the technology has taken time.
The field for VADs has been subjected to a continuum of technological upgrades. A classic example would be the illustration of the HeartMate family of devices. The HeartMate I is a pneumatic pump that has been in use since 1986, whose electronic version was released in 1992 and has since then technologically evolved. This device has been looked to as a standard of care against which all other devices are compared. HeartMate II is an axial–continuous flow pump whose design eliminates the need for valves. This device, manufactured by Thoratec Corp. and recently FDA cleared to be used as a bridge to transplant, marks an important technological advancement in the field. Heartmate II, smaller than a D-cell battery, is the first in a new generation of products that circulate blood using a small spinning blade. According to analysts, HeartMate II may generate $130 million a year by 2010. Now with the HeartMate III currently under development, another advance in VADs will manifest in a centrifugal-continuous flow pump that is suspended magnetically, offering patients longer durations of support.
But Heartmate II or III cannot rest on its market dominance laurels with devices from Ventracor Ltd., World Heart Corp. and HeartWare Ltd. all are entering final clinical trials this year. Reportedly, these devices may be easier to use than Thoratec’s model. Plus, another bridge to recovery VAD, the Impella 2.5 Cardiac Assist Device by Abiomed Inc., recently received FDA clearance for use under the 510(k) for partial circulatory support up to six hours. This was along with the intra-aortic balloon pump (IABP), which also has 510(k) clearance.
The Impella 2.5 is inserted percutaneously in the catheterization laboratory via the femoral artery into the left ventricle. Up to 2.5 liters of blood per minute are delivered by the pump from the left ventricle into the ascending aorta, providing the heart with active support in critical situations.
“FDA clearance of the Abiomed Impella 2.5 represents the next step in enabling heart recovery for patients in the U.S. and will likely change the standard of care in the catheterization lab,” said Abiomed Chairman, CEO and President Michael R. Minogue. “The device seamlessly provides immediate, minimally invasive circulatory support for critical patients.”
The new VAD is now approved in more than 40 countries, including in Europe for up to seven days of support under the CE Mark. Sales sales alone for the Impella 2.5 could generate revenues on par with the $58.4 million Abiomed earned in 2007, according to Greg Simpson, an analyst at Stifel Nicolaus. Simpson estimates that the device will bring $50 million in sales by 2009.
Understanding the fact that one device would not suit the requirements for all, manufacturers are now looking at developing products for women and children. Every year an estimated 1,000 children require VAD support. The DeBakey VAD Child has obtained Humanitarian Device Exemption (HDE) to support pediatric patients aged between 5 and 16. Companies like WorldHeart Corp. are involved in the development of devices to cater to young patients.
In the future, expect to see devices that will address the current gap in treating pediatric patients, helping them live longer.



 June 19, 2024
June 19, 2024