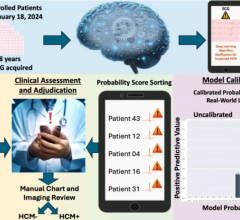
An example of artificial intelligence-aided clinical decision support software for a heart failure patient from the vendor HealthReveal. The AI pulled in relevant patient data from the electronic medical record and offers recommendations for care based on current American Heart Association (AHA) guidelines. It also offers the citations for where to find the guidelines and prescribing information for the recommended drug.
The consistent provision of guideline-directed medical therapy (GDMT) — care delivered according to established guidelines and safety standards — is crucial for every healthcare encounter, especially when treating patients with chronic disease. Chronic diseases are “among the most common, costly, and preventable of all health problems,” according to the Centers for Disease Control (CDC).[1] About half of all U.S. adults suffer from one or more chronic diseases, and 86 percent of the United States’ $2.7 trillion annual healthcare expenditures are the result of chronic illness. Treating these patients optimally would presumably be a priority for our system.
Remarkably, patients afflicted with chronic conditions often do not receive guideline-directed care. One study published in the New England Journal of Medicine (NEJM) found that almost half — 46.3 percent — of chronically ill participants “did not receive recommended care.”[2] Furthermore, failure to deploy validated evidence represents a pervasive failing of our healthcare system. Another study published in the Journal of the American Medical Association (JAMA) confirmed that rates of recommended medical treatments were low and remained essentially unchanged from 2002 to 2013, despite relatively high rates providing recommended diagnostic and preventative care over the same time period.[3]
Examining the Persistent Failure to Follow the Evidence
Examples of the costly, and lethal, consequences of failing to utilize GDMT are numerous. A study in the March 2017 issue of JAMA found that among nearly 95,000 patients with a known history of atrial fibrillation (AF) who had an acute ischemic stroke, an astonishing 83 percent “were not receiving therapeutic anticoagulation prior to stroke.”[4] This was not a case of patient non-adherence, but rather of physicians never having prescribed the medication or failing to adjust drug dosages for individual patients. Consider the avoidable suffering and savings resulting from pre-empting these strokes, had the patients received optimal therapeutic interventions.
More recently, a study in the July 2018 issue of the Journal of the American College of Cardiology (JACC) explored the use of GDMT in patients with heart failure with reduced ejection fraction (HFrEF), one of the leading causes of admission/readmission in Medicare. While nothing that “guidelines strongly recommend patients with HFrEF be treated with multiple medications proven to improve clinical outcomes,” the study revealed that this was not occurring in real-world settings.[5]
“Among eligible patients, 27%, 33%, and 67% were not prescribed ACEI/ARB/ARNI, beta-blocker, and MRA therapy, respectively,” the study authors wrote. “When medications were prescribed, few patients were receiving target doses of ACEI/ARB (17%), ARNI (14%), and beta-blocker (28%) … Among patients eligible for all classes of medication, 1% were simultaneously receiving target doses of ACE/ARB/ARNI, beta-blocker, and MRA.”
The study authors concluded, “Strategies to improve guideline-directed use of HFrEF medications remain urgently needed.”
The Limitations of the Human Mind
Physicians face a number of challenges when it comes to delivering care in today’s fast-paced environment, including the pressures of transitioning from fee-for-service to value-based care, coping with health information technology, patient data overload, and an explosion of new medical knowledge. A clinician’s ability to access and synthesize enormous volumes of data and then translate that data to actionable, patient-specific interventions consistent with complex, evolving guidelines, tests the limits of even the best and brightest of human minds.
Doctors Ziad Obermeyer and Thomas H. Lee illustrate the problem in their NEJM perspectives article titled, “Lost in Thought — The Limits of the Human Mind and the Future of Medicine,”[6] as follows: “Medical knowledge is expanding rapidly, with a widening array of therapies and diagnostics fueled by advances in immunology, genetics, and systems biology. Patients are older, with more coexisting illnesses and more medications. They see more specialists and undergo more diagnostic testing, which leads to exponential accumulation of electronic health record (EHR) data. Every patient is now a “big data” challenge, with vast amounts of information on past trajectories and current states…”
The authors observe “the complexity of medicine now exceeds the capacity of the human mind.” However, technological advances will provide the solution the authors wrote.
“But there is hope,” they wrote. “The same computers that today torment us with never-ending checkboxes and forms will tomorrow be able to process and synthesize medical data in ways we could never do ourselves. Already, there are indications that data science can help us with critical problems.”
Fortunately, we live in an era where AI and machine learning can help solve these problems.
Bridging GDMT and Patient Data, Enhancing with AI and ML
Through the advances of AI and machine learning, the healthcare industry now has the capability to bring GDMT directly to clinicians and patients at the moment they need it to make personalized care decisions based on real-time patient data.
“We are no longer on the brink of change resulting from AI — we are already immersed in a world with software-driven machines learning to process unstructured information in meaningful ways; something that until relatively recently was the domain of humans alone,” according to a report from technology consulting firm Infosys released in January 2018, titled “Leadership in the Age of AI.”[7] Of 1,000 business and IT decision makers surveyed for the Infosys report, 51 percent of those in the healthcare industry said their organizations are already experiencing disruption due to AI, while 71 percent of those in the healthcare industry “strongly or somewhat agreed” that their future business plans will be informed and transformed by the development of AI technology.
And a 2016 study from Frost & Sullivan projected a 40 percent growth rate in the market for AI in healthcare between 2016 and 2021.[8] The healthcare consulting company noting that AI has the potential to improve outcomes by 30 to 40 percent while at the same time reducing the costs of treatment by as much as 50 percent.
An example of how AI can work to deliver immediate access to guides is the HealthReveal software, It creates a “digital replica” of each patient, incorporating data from electronic health records, payers and even patient-generated health data (PGHD) from remote monitoring technology (devices that are wearable or implantable, or can be used in the home), such as blood pressure readings and blood sugar tests. From there, using cloud-based technology, the data collected about specific patients can be compared against the latest evidence-based guidelines. As discrepancies emerge, customized, real-time recommendations can be delivered instantaneously to the clinician, caregiver, or to the patient directly, alerting them to the likelihood of adverse events, and most importantly, offering actionable interventions for care to prevent those events from occurring.
A June 2017 report from McKinsey Global Institute confirms the impact AI can have on patient care and outcomes, as well as on healthcare costs.[9] The report says, “Healthcare is a promising market for AI … AI has the potential to help doctors improve their diagnoses, forecast the spread of diseases, and customize treatments. Artificial intelligence combined with health care digitization can … transform the way we treat the chronic diseases that account for a large share of health-care budgets. Indeed … AI tools will enable healthcare to dramatically accelerate its shift toward preventive medicine.”
AI in healthcare is no longer a promise for the future – it’s a promise for today.
Editor’s note: Lonny Reisman, M.D., is founder and CEO of HealthReveal. He is a recognized leader in health information technology, patient safety and evidence-based medicine. Prior to working at HealthReveal, he was CEO and co-founder of ActiveHealth Management, now an Aetna subsidiary, following nearly 20 years of experience as a physician and consultant to large employers. Reisman was an attending physician at New York Hospital and St. Luke’s-Roosevelt Hospital Center between 1987 and 1999, and was a cardiology fellow at the University of Chicago from 1985 to 1987. He received his medical degree from Tel Aviv University. You can reach him at [email protected]
References:


 September 24, 2025
September 24, 2025