Kim Phelan, Editor
At a pivotal time of advancement in cardiovascular imaging, diagnostics, interventions and therapies, a time when specialty heart hospitals are forming to combat the deadliest disease in America, the federal purse strings are about to be pulled a little tighter in 2007, and rules for these types of narrowly focused hospitals are going to be more stringent.
The Centers for Medicare and Medicaid (CMS) have announced in a final report that specialty hospitals that fail to report their financial structure to the federal government will be fined $10,000 per day. These hospitals will also be required to disclose to patients their financial relationships with physicians, and must treat all emergency cases regardless of patients’ ability to pay. CMS, according to an article published on Modernhealthcare.com, has allowed a federal moratorium on Medicare payments to new specialty hospitals to lapse as of August 8.
But there’s more bad news for cardiologists as well as other physicians.
Doctors are about to take a pay cut as Medicare prepares to reduce physician reimbursement rates by 5.1 percent, a plan scheduled, under current law, to take effect in 2007. But Medicare will spend about $61.5 billion on physician services next year, under the proposed physician fee schedule, Modernhealthcare reports.
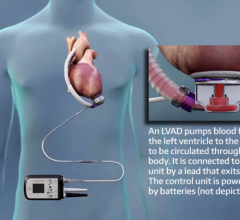
The reimbursement landscape may not be lush, but it isn’t entirely bleak either. While investigating some of the latest thinking on ventricular assist devices for a feature story we present on page 58, I learned from Mike Minogue, CEO of Abiomed, that CMS was persuaded last fall to change its view on reimbursing devices used to recover patients’ hearts. According to Minogue, the agency granted approval on Oct. 1, 2005 for heart recovery devices equal to heart transplant, meaning that for the implant and explant of a VAD, the hospital receives a DRG 103, the heart transplantation reimbursement.
I asked a spokesperson for Thoratec whether reimbursement is more favorable today for certain devices than for others, to which she replied: “For cardiologists, reimbursement is consistent regardless of the device implanted. Patient length of stay affects the amount of visits and payment in the inpatient setting.”
Devices and procedures that cardiologists bring to their patients are undeniably expensive. Physicians make heavy decisions every day about treatment path and treatment timing, weighing what’s right for the patient as well as the costs that will be involved. Dr. Leslie Miller at Georgetown University and Washington Hospital told me that doctors must sometimes discern whether patients receiving devices are likely to experience “meaningful recovery.”
In the end, despite the push and pull of reimbursement policies, physicians receive an invaluable reward in exchange for the burdens they carry.
“We are trying to be very good stewards of expensive resource[s],” said Dr. Miller. “We have seen people’s lives totally turned around, and there are very few things in medicine more gratifying than heart transplantation or a successful mechanical device because these people don’t just survive. They can truly regain function capacity, integrating with their families, [even] going back to work — really having a categorical life. And if it is yours, how do you put a dollar value on that?”
You can’t.
Thanks for reading this special TCT edition!


 June 19, 2024
June 19, 2024