September 23, 2013 — Cardiologists are increasingly accessing coronary arteries by way of the wrist rather than the groin to insert life-saving stents into patients with blocked arteries, according to the first broad report of the American College of Cardiology’s clinical data registries published online in the Journal of the American College of Cardiology.
The report, “Cardiovascular Care Facts: A Report from the National Cardiovascular Data Registry ? 2011,” includes data about stents from the CathPCI Registry, the ACC’s national database of hospital records on stenting and angioplasty, as well a wide range of data from the other four ACC National Cardiovascular Data Registries for which comprehensive data from 2011 are available.
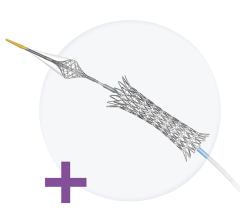
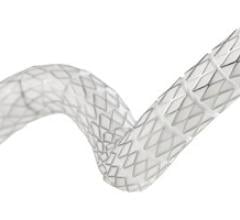
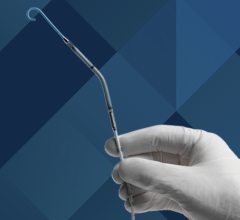
The report showed stenting (percutaneous coronary intervention or PCI) performed at the radial access site (the wrist) increased from 2.9 percent of cases in 2009 to 10.9 percent of cases in 2011, while stenting performed at the femoral access site (the groin) decreased from 96.5 percent to 88.8 percent during the same time period. While this approach is new and still being studied, research has shown that radial access can reduce the risk of complications, discomfort and recovery times in some patients. The report suggests that clinicians who perform PCI are becoming more comfortable with this approach and it is becoming more commonly used.
"The data in this report demonstrate the value of national registries in providing an unprecedented and broad perspective on the care and outcomes of patients with cardiovascular disease,” said Frederick Masoudi, M.D., MSP, senior medical officer of the NCDR. “These registries are key tools in understanding and improving care for cardiovascular patients across the United States."
Other top findings from the report outline several successes in heart disease care as well as opportunities for further improving a patient’s treatment and follow-up care experience.
There have been continued improvements in meeting guideline-recommended door-to-balloon (D2B) times of 90 minutes or less for patients with ST-segment elevation myocardial infarction. In the ACTION-GWTG Registry alone, the proportion of patients with D2B times of 90 minutes or less for non-transfer patients increased from 81 percent in 2008 to 94.2 percent in 2011, while among patients who were transferred for percutaneous coronary intervention (PCI) this proportion increased from 18 percent in 2008 to 30.4 percent in 2011.
Findings from the CathPCI Registry show providers are consistently prescribing optimal medical therapy, including aspirin, thienopyridine/P2Y12 inhibitor, lipid lowering agents and beta-blockers, at discharge for PCI patients. Prescription of aspirin and thienopyridine at discharge have remained relatively steady between 96 percent and 98 percent between 2009 and 2011, while prescriptions of lipid lowering agents and beta blockers have increased. Prescription of lipid lowering agents rose from 89.7 percent in 2009 to 92.5 percent in 2011. Beta blocker prescriptions have increased from 83.1 percent to 86.3 percent.
In the PINNACLE Registry, data show there continues to be an opportunity for increased education for patients and clinicians about optimal anticoagulation strategies for stroke prevention in atrial fibrillation, as 57.2 percent of eligible patients with atrial fibrillation were prescribed anticoagulation therapy.
The ICD Registry identifies an opportunity for the use of medical therapy for patients with prior myocardial infarction or left ventricular systolic dysfunction; nearly 25 percent of ICD patients did not receive optimal medical therapy with ACE inhibitors and/or beta blockers at discharge.
PINNACLE Registry data overwhelmingly shows providers regularly recording patient blood pressures (95.1 percent), only a minority (34.5 percent) of providers are taking things a step further and implementing hypertension care plans.
According to CathPCI Registry data, opportunities exist to improve not only adherence to appropriate use criteria in patients without acute coronary syndrome (ACS) but potentially clarify areas of uncertainty. While a little more than half of patients without ACS (52.8 percent) were evaluated appropriately for PCI procedures, 37.3 percent fell into the uncertain category, while nearly 10 percent were inappropriate. In contrast, patients with ACS were appropriately evaluated for PCI procedures 99.1 percent of the time.
For more information: cardiosource.org/ACC


 November 24, 2025
November 24, 2025