
The cath lab staff UH Portage Medical Center.
Primary percutaneous coronary intervention (PCI) is the preferred treatment for acute ST-segment elevation myocardial infarction (STEMI). Previous studies have shown a strong association between urgent performance of primary PCI, as assessed in terms of the door-to-balloon time (D2B), the interval from the patient's arrival at the hospital to inflation of the balloon to restore flow, and reduced mortality. To reduce D2B times to improve patient outcomes, University Hospitals Portage Medical Center, a community hospital serving Portage County, Ohio, developed a close partnership with its emergency medical services (EMS), emergency department (ER) and the cath lab. The collaboration has cut proven D2B times by more than half and recently helped achieve a nine-minute door-to-balloon time.
Current joint clinical practice guidelines of the American College of Cardiology (ACC) and the American Heart Association (AHA) recommend a door-to-balloon time of 90 minutes or less as the goal, giving it a Class I (highest level) recommendation. Because of this recommendation, door-to-balloon time has become the focus of local, regional, and national quality-improvement initiatives and is currently tracked by a number of clinical registries. Consequently, door-to-balloon times are now publicly reported, and the percentage of patients for whom the door-to-balloon time is 90 minutes or less has evolved into a key quality metric. Institutional D2B times also have financial implications, since they are now tied to reimbursement from the Centers for Medicare and Medicaid Services (CMS).
At UH Portage Medical Center, we started a coronary interventional program in December 2016 after obtaining special permission from the Ohio Department of Health to be an interventional center without surgical backup. Our average door-to-balloon time, including transfer before starting the program, was 119 minutes. We had to transport all the patients from our emergency room (ER) to a tertiary care center by helicopter and average cost per case for transportation was $36,000.
Coordinating STEMI Care With EMS, Cath Lab
When we started the coronary interventional program at Portage, we partnered with the local EMS system in Ravenna City and surrounding communities. We developed a coordinated STEMI care model with standardized protocols for prehospital activation of the cardiac catheterization lab. The protocol calls for EMS to administer aspirin and a loading dose of ticragrelor and heparin in the field.
The ECG from the field is transmitted electronically to the ER, and a central paging system is initiated by the ER nurse or physician. This sends a text message to the on-call cath lab team and the interventional cardiologist. The interventional cardiologist on-call phones back the ER within five minutes.
Once there is confirmation of a STEMI diagnosis based on the ECG and report from EMS we bring the patient directly to the cath lab from the ambulance, bypassing the ER. A focused history and physical examination is done on the way to the cath lab.
We also hold educational sessions in the local community in partnership with the local EMS to educate people about signs and symptoms of heart attack, how to call for help in emergency, as well as prevention and screening for heart disease. We do give regular feedback to the EMS systems about their care prior to transporting the patient to the hospital and give them the opportunity to watch the cases in the cath lab. We consider the EMS system as an essential part of the heart care team to achieve optimal standards of care in the STEMI patients.
Using these protocols, we now have average door-to-balloon times of 47 minutes. This includes day and nighttime activations (when the team has to come from home).
Case Report Example of a Nine-Minute D2B Time
The protocols used by UH Portage Medical Center recently helped achieve a nine-minute door-to-balloon time in the cath lab.
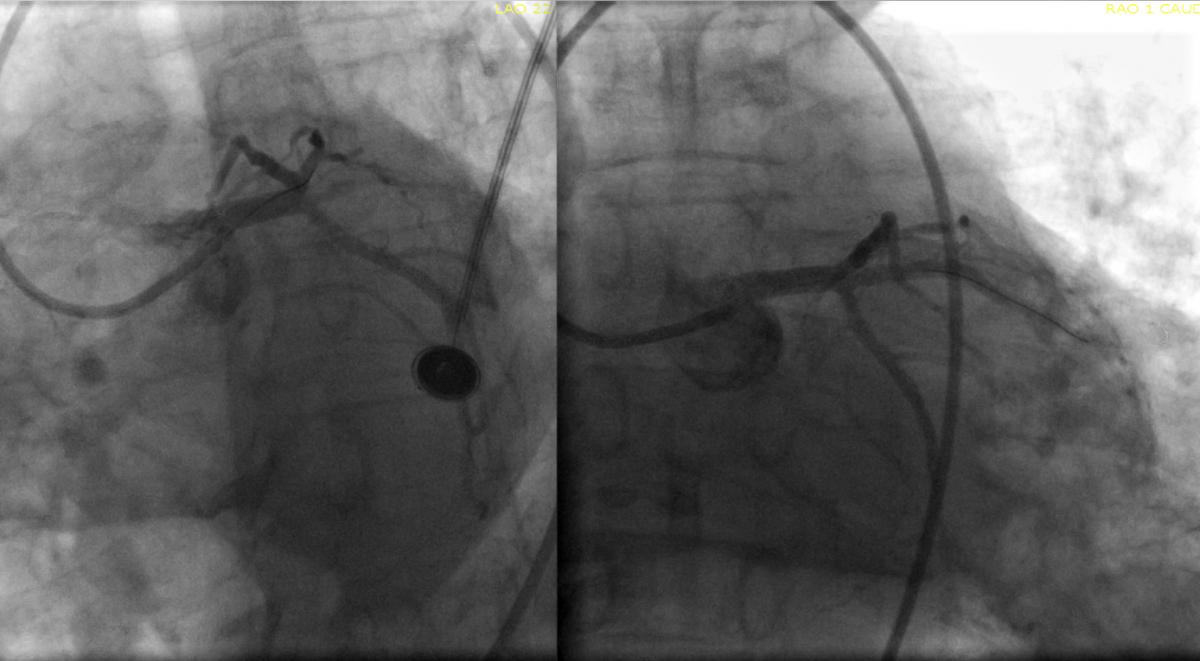
Comparison of a STEMI coronary artery blockage pre- and post-PCI for a patient who had a 9-minute door-to-balloon time. An 83-year-old male patient with a medical history of significant hypertension and dyslipidemia started having severe chest pain described as pressure radiating to his arm associated with diaphoresis at home. He called 911 and EMS was activated. Upon arrival to home, EMS did an ECG on the patient, which confirmed an infero-posterior myocardial infarction (MI) and transmitted the ECG to UH Portage Medical Center ER for confirmation to activate the cath lab. See more images from this case below the article.
An 83-year-old male patient with a medical history of significant hypertension and dyslipidemia started having severe chest pain described as pressure radiating to his arm associated with diaphoresis at home. He called 911 and EMS was activated. Upon arrival to home, Streetsboro EMS (a local city in Portage County) did an ECG on the patient, which confirmed an infero-posterior myocardial infarction (MI) and transmitted the ECG to UH Portage Medical Center.
Upon confirmation by an ER physician, the STEMI protocol was initiated and the cath lab was activated. The cath lab staff and the interventional cardiologist received the patient in the ambulance bay and he was taken straight to the cath lab.
Vascular access was obtained using a Launcher EBU3.5 guiding catheter. A left coronary angiogram was obtained, which revealed a totally occluded ramus intermedius (RI) artery with large clot burden. The lesion was crossed with a Whisper wire and mechanical aspiration thrombectomy was performed with a Penumbra catheter (CATRx). This established flow in the RI and primary stenting was performed with a Xience Sierra 3.0 x 23 mm long drug-eluting stent (DES). The DES was post-dilated with a 3.0 x 15 noncompliant balloon. The door-to-device (balloon) time was 9 minutes. There was immediate resolution of the patient’s symptoms and ST-segment elevation.
This case illustrates how we can optimize STEMI care by coordinated protocols and partnerships between EMS systems and hospitals to improve the quality of care we provide to these acutely ill patients in the community.
Editor's Note: Anjan Gupta, M.D., FACC, FSCAI, is director of the cath lab at the University Hospitals Portage Medical Center in Ravenna, Ohio. He has expertise in critical limb ischemia, high-risk PCI, peripheral vascular diseases (PAD) and preventive cardiology. Read more about his work on the D2B protocol at Portage Medical Center.






 November 14, 2025
November 14, 2025 









