TrueView allows the user to locate the optimum viewing angle for the lesion and bifurcation.
When it comes to diagnosing heart disease, highly detailed 3D images of a coronary artery comes to mind. But advanced imaging has expanded its role in the cath lab beyond diagnosis, as 3D images are used to guide physicians through interventional procedures. But what it taking imaging in the cath lab to the next generation is 4D imaging, in its truest sense. 4D imaging will project a cine view as clinicians move through the body in real time.
Beyond two dimensional viewing
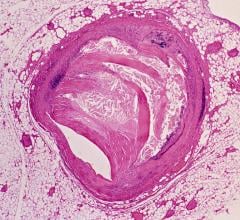
Many interventional cardiologists face the daily challenge of assessing and treating potentially life-threatening heart conditions without a clear picture of the coronary vessels. Often times, 2D imaging misrepresents lesion lengths and overlapping branches in bifurcations. In addition to visualization challenges, interventional cardiologists must also perform complex procedures, as quickly as possible, and with a minimum radiation dose.
“The heart and the coronaries are 3D/4D objects and the medical imaging is finally catching up to the realities of the anatomy,” said John Carroll M.D., director of the Cardiac and Vascular Center at the University of Colorado Hospital in Denver. “We’re getting past the medical imaging constraints of the past, which were two- dimension projections of slice images, which really are a burden because you have to take two images and process them in your own brain to really understand that you are looking at a 3D object.”
Three-dimensional imaging assists interventionalists in solving several imaging tasks in the world of coronary imaging. As opposed to two-dimensional imaging, it allows cardiologists to determine optimal views, minimizes lesion foreshortening and prevents overlap with surrounding vessels.
“[3D/4D] is becoming more prevalent in different modalities and its being incorporated in the cath lab mainly to facilitate interventional therapy, including both coronary and vascular interventions, but also structural heart disease interventions,” said Dr. Carroll.
Workflow systems, such as the Allura 3D-CA by Philips Medical Systems, serve as visual planning and interventional tools that provide accurate 3D models of the coronary arteries. The Allura 3D-CA assists cardiologists in getting an accurate view of the patient on the first try by creating a 3D model of the coronary arteries. The system starts with a four-second rotational scan and selects image frames from the same cardiac phase. In the control room, the user then chooses two images with more than 30 degrees difference in angulation, and the Allura assists in marking the artery’s area of interest in the two selected images.
With this information, the Allura 3D-CA produces a 3D model of the artery that can be viewed and controlled tableside. According to Dr. Carroll, visualization tools such as the Philips Allura 3D-CA improve outcomes by reducing the radiation dose and contrast volume that patients receive by allowing cardiologists to more efficiently take images, process them into three dimensions and “get away from the traditional method of taking many pictures from different angles until you get the entire picture.” This method also drastically reduces time spent acquiring accurate 3D models.
“The bottom line is that when we work more efficiently, use less contrast and radiation and have greater confidence, we are optimizing our results,” said Dr. Carroll.
This 3D image can be viewed from any perspective as the user controls rotation, panning and zooming features. The Allura’s TrueView Map feature allows the user to locate the optimum viewing angle for the lesion and bifurcation, and a real-time link between the TrueView and the C-arm keeps the model and the angulation synchronized throughout the procedure, reportedly optimizing speed and accuracy in stand positioning.
“We certainly use 3D coronary models in complex interventions, where understanding the three-dimensional relationships and understanding 3D properties of coronary arteries like curvature and bifurcation angles and exact lesion length is very important,” said Dr. Carroll. “You can only get that quantified if you’ve got the person’s coronary arteries in a 3D format.”
Putting the pieces together
At the University of Colorado Hospital, Dr. Carroll uses an Allura 3D-CA, Allura Xper FD-20 and Allura Xper FD10/10 system from Philips for cardiac procedures. Each has a workstation that allows 3D CA and has the TrueView functionality. The FD-20 also has EP Navigator that allows cardiologists to overlay live fluoroscopy to previously acquired cardiac CT images. The FD-20 system also has StentBoost, C-Arm Follow and all of Dr. Carroll’s research acquisition prototypes, including dual-axis rotational angiography and 180-degree rotational acquisitions with gated 3D reconstruction.
“The C-Arm Follow puts up either the cardiac CT data or a 3D model of the coronary arteries on a separate display screen in front of the interventionalist, and whenever we move the gantry, the 3D model follows exactly,” said Dr. Carroll. “So before you take a picture you are able to know what it is going to look like.”
StentBoost is a tool designed to improve visualization of stents in the coronary arteries during interventions. It enables interventionalists to see the stent and vessel in the same image, which reportedly helps position stents more accurately in side branches. By viewing the stent and vessel in the same image, StentBoost helps cardiologists instantly see underdeployment and malapposition and helps them to position the balloon. It also helps identify stent fractures or gaps between stents and correct them during the procedure.
“Recently, we have added three-dimensional transesophageal echo for guidance of structural heart disease interventions and that has really changed things dramatically because it is real-time 3D imaging,” said Dr. Carroll. “For the first time ever we are doing catheter manipulations in 3D space and actually looking at the 3D image. Technically it is in 4D because it is a moving image.”
Embracing the fourth dimension
In order for the average cath lab to process the large amounts of data required for 4D imaging, they are going to need powerful technology. To solve this problem, cardiologists of the future may use graphics processing units (GPU) for 4D cardiac MR and ultrasound images.
According to Roy Eagleson, Ph.D., Professor of Electrical and Computer Engineering at The University of Western Ontario, clinicians and researchers alike make use of software applications, which make heavy demands on computer workstation CPU resources. Modern graphics cards are designed to handle the computations involved in displaying geometries and texture, and since these computations can be parallelized, modern cards have been designed with GPUs that have multiple processing cores.
Although four-dimensional images, which consist of three dimensions plus a time element, are not yet completely available for coronary imaging, Dr. Carroll believes that such imaging and viewing capabilities will emerge as the next generation in advanced imaging applications.
“4D is important in all cardiac work because the heart is obviously very dynamic and many of our problems, both diagnostic and interventional, are related to motion,” said Dr. Carroll.



 October 24, 2025
October 24, 2025