
FDA Clears First Drug Coated Balloon
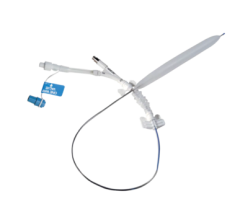
October 13, 2014 — C. R. Bard Inc. announced the U.S. Food and Drug Administration (FDA) approval of the Lutonix 035 drug-coated balloon (DCB) catheter for percutaneous transluminal angioplasty (PTA) after pre-dilatation, for the treatment of de novo or restenotic lesions up to 150 mm in length in native vascular disease of the superficial femoral or popliteal arteries with reference vessel diameters of 4-6 mm. This approval follows a unanimous favorable recommendation from the FDA’s Circulatory Systems Devices Advisory Panel in June 2014. The Lutonix 035 DCB — the first and only FDA-approved DCB in the United States — is an angioplasty balloon coated with a therapeutic dose of the drug paclitaxel, and also utilizes standard mechanical dilatation of the vessel to restore blood flow for patients with peripheral arterial disease (PAD) in the femoropopliteal arteries.
FDA approval of the Lutonix 035 DCB was supported by results of the LEVANT 2 pivotal study, a global, prospective, single-blind, randomized, 54-site study (42 sites in the U.S. and 12 in Europe) that enrolled all patients under one protocol. At one year, the LEVANT 2 study demonstrated improved patency of the Lutonix 035 DCB compared to standard PTA: 73.5 percent vs. 56.8 percent, p<0.001 by Kaplan-Meier time-to-event analysis. It also demonstrated clinical benefits of sustained improvement in Rutherford Class and improved walking distance scores. The LEVANT 2 study followed a rigorous blinding protocol designed to reduce bias in the results to accurately and scientifically assess and compare the long-term performance of key clinical measures. The LEVANT clinical program, which includes registry data, enrolled more than 1,000 patients and demonstrated robust safety of the device comparable to PTA, including the same low rate of distal embolic events and rate of reintervention for thrombotic events.
“The Lutonix 035 DCB provides physicians with an opportunity to enhance the treatment protocol for patients with occlusive disease of the femoropopliteal artery with a safe, effective method of delivering paclitaxel directly to stenosed vessels,” said Kenneth Rosenfield, M.D., section head, vascular medicine and intervention chairman, Massachusetts General Hospital, professor of medicine, Harvard University School of Medicine, and LEVANT 2 principal investigator. “This DCB is a new first-line therapy for treating blockages, without closing the door to other treatment options down the road. I envision also using the Lutonix 035 DCB to complement existing therapy options.”
The American Heart Association (AHA) estimates that PAD, a life-threatening condition, affects at least 8 million Americans by narrowing arteries and reducing blood flow to the limbs.[1] Patients with PAD in the femoropopliteal arteries are at risk for lower-extremity amputation, particularly in people over the age of 50.[2] Successful treatment of PAD in the femoropopliteal arteries requires improved blood flow (patency) for longer periods of time. While there are both noninvasive and invasive treatment options for these arteries available, each has associated limitations. PTA is currently the first-line, standard-of-care treatment for PAD, according to the American College of Cardiology (ACC) and AHA 2011 guidelines; however, it is limited by its relative lack of long-term patency.
“In line with Bard’s commitment to delivering products that improve patient care, we are proud to offer another Bard first-of-its-kind innovation that expands therapy options for this painful, progressive and debilitating disease,” said Timothy M. Ring, chairman and CEO of C. R. Bard. “The Lutonix 035 DCB gives clinicians another option as they seek to provide prolonged patency to patients confronted with femoropopliteal occlusive disease.”
The Lutonix 035 DCB has been available commercially in Europe since 2012.
For more information: www.crbard.com
References:
1. Why PAD Matters – American Heart Association Web site. Available at:http://www.heart.org/HEARTORG/Conditions/More/PeripheralArteryDisease/Why-PAD-Matters_UCM_301303_Article.jsp.
2. Peripheral Arterial Disease – NIH National Heart, Lung, and Blood Institute. Available at: https://www.nhlbi.nih.gov/health/health-topics/topics/pad.

 June 13, 2024
June 13, 2024 








